Dott.ssa Silvia Baccini, fisioterapista, Master riabilitazione del pavimento pelvico
Dott.ssa Cantù Daniela
A questionnaire based on the most recent evidence about pelvic organs prolapse has been
created and issued to a pool of physiotherapists specialised in pelvic floor rehabilitation.
The final goal is to compare all of the data available in literature with the actual
professional clinical execution.
Research on the latest POP rehabilitation revisions has been performed, together with
analysing guidelines and RCT which have been published on the PubMed platform
between the years 2020 and 2023. Based on its results, a list of 22 questions, subdivided
into 4 main topics, has been drawn up: 1) competencies, training and clinical experience of
the physiotherapist; 2) profile of the patient with POP who receives the physiotherapeutic
treatment; 3) treatment tools and techniques; 4) outcome and modality of its achievement;
5) pre and post surgery physiotherapy. The data gathered has finally been discussed and
compared to the relevant evidence outlined in specialised literature.
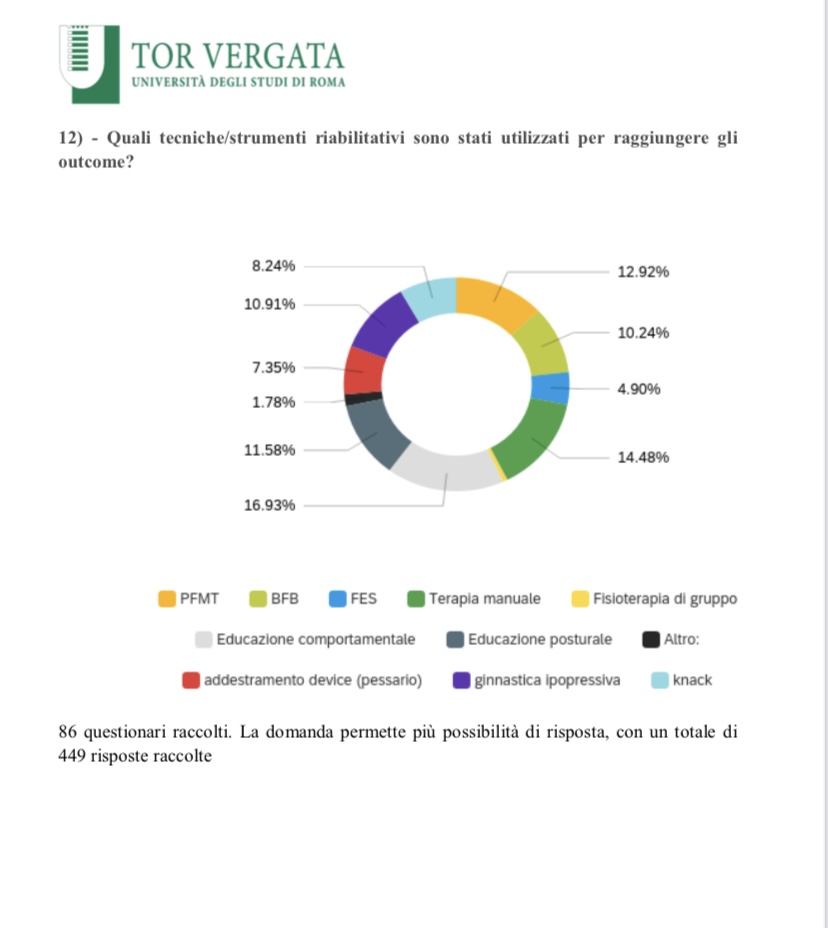
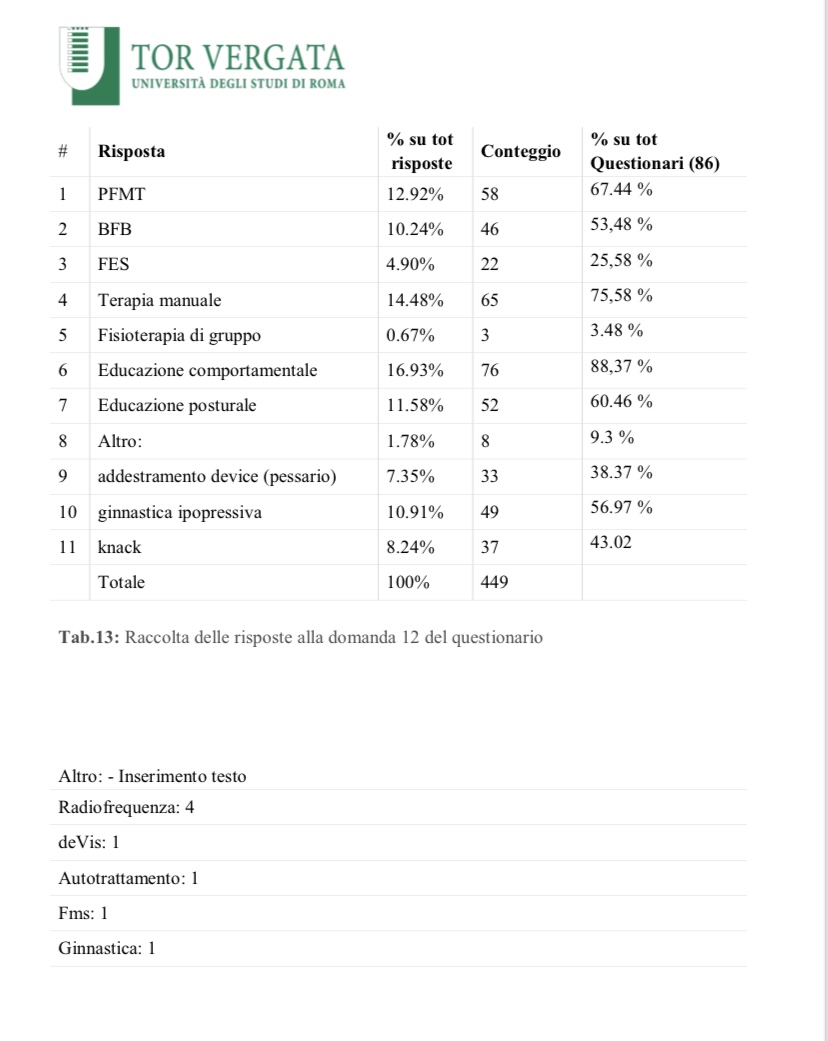
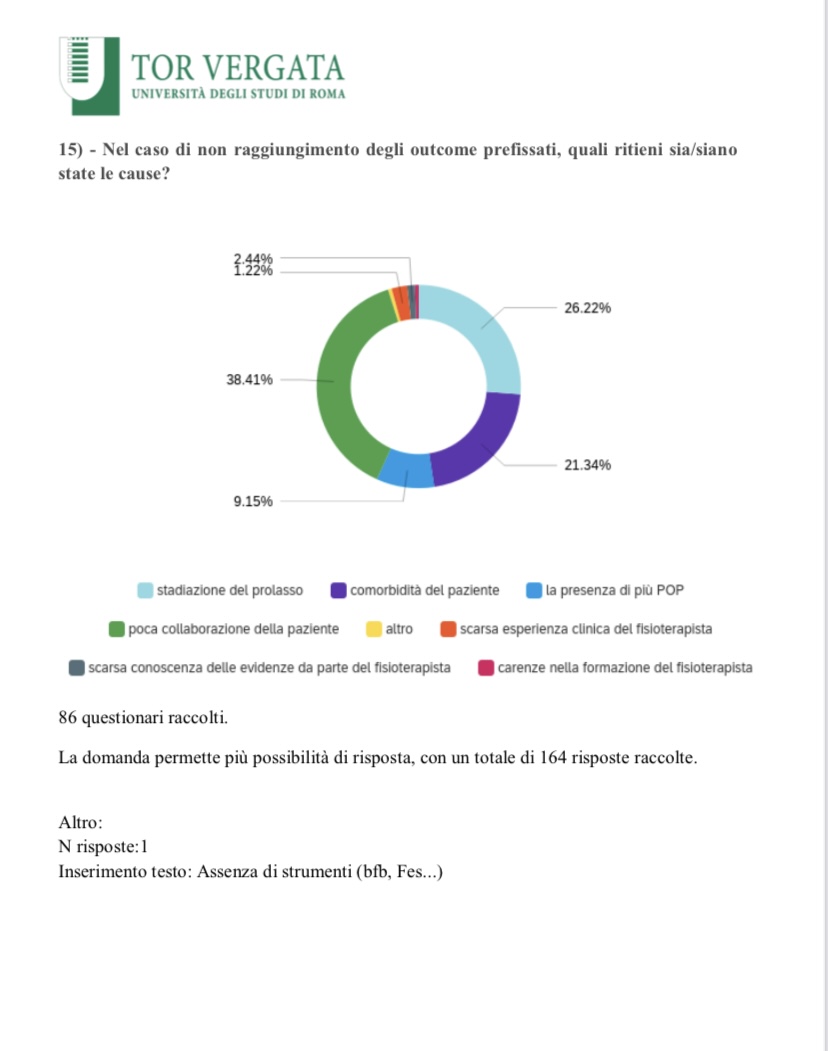
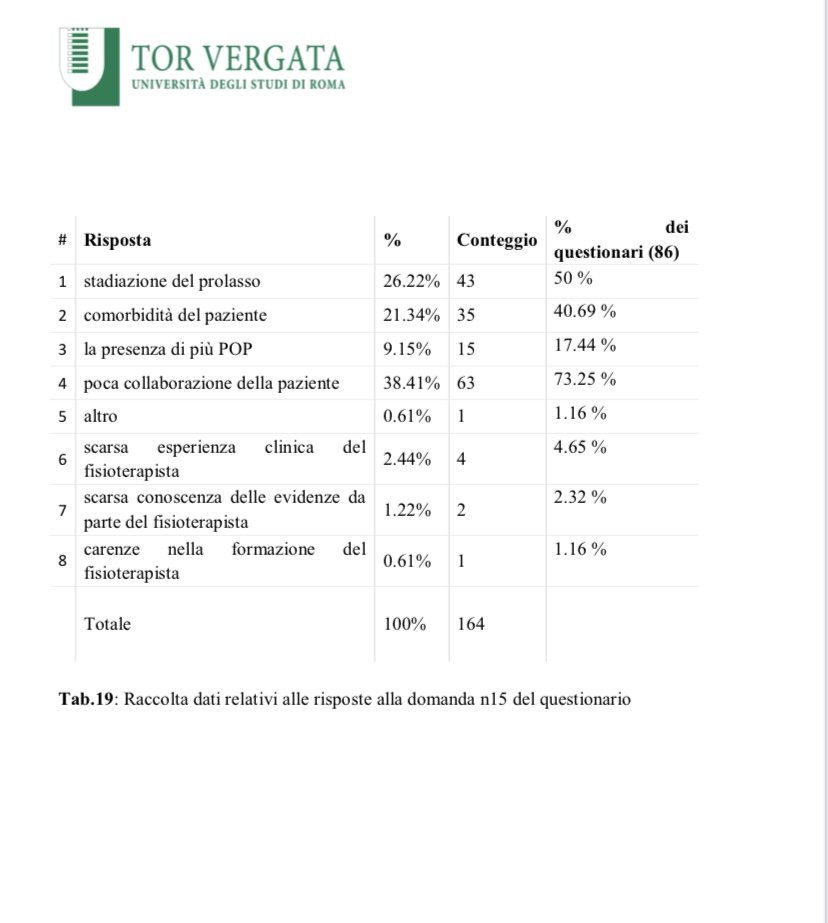
The questionnaire has been filled out by 86 physiotherapists who are either expert or
specialised in pelvic floor rehabilitation. The collected data has been compared both with
guidelines and the most recent articles issued in relation to the physiotherapeutic treatment
of patients affected by POP. The data concerning the choices of treatment has come out to
be different compared to what it would have been expected based on the evidence in
literature. The choice to use PFMT as a treatment technique for POP patients’
rehabilitation, has involved 67% of the physiotherapists. This percentage has been rather
unexpected considering that popular guidelines such as NICE 2019 recommend it as an
option for patients affected by POP. Also, other figures emerged to be in disagreement
with the current literature: this is the case of hypopressive exercise and the use of pessary.
The future objective would be to implement qualitative and meaningful studies and
research in order to recognise the effectiveness of physical rehabilitative techniques for
POP patients, including radiofrequency and hypopressive exercise, for which there is not
much evidence still.
It is necessary to strengthen studies and scientific evidence of the rehabilitative treatment
applied in prevention of post-surgery relapse. Currently, there are no studies that can
compare the long-term outcome preservation within groups of patients with prolapse
setbacks, who have been treated with physiotherapy both before and after surgery, versus
similar patients who have not undergone a physiotherapeutic cycle. Another relevant piece
of data is about physiotherapists proposing pessary as a treatment option: only a very
minimal percentage of colleagues do so. It is crucial to identify the reasons behind this, in
light of the large amount of literature in support of the many benefits and advantages of
this therapy option.
ibliografia
1. 1«Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A,
Petri E, Rizk DE, Sand PK, Schaer GN; International Urogynecological
Association; International Continence Society. An International Urogynecological
Association (IUGA)/International Continence Society (ICS) joint report on the
terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4-
20. doi: 10.1002/nau.20798. PMID: 19941278.»
2. «Prolapsus génital de la femme – Des solutions pour le traiter». HAS ( Haute
Autoritè de Santeè), april 2022. https://www.has-
sante.fr/jcms/p_3337359/fr/prolapsus-genital-de-la-femme-des-solutions-pour-le-
traiter.
3. Raju R, Linder BJ. Evaluation and Management of Pelvic Organ Prolapse. Mayo
Clin Proc. 2021 Dec;96(12):3122-3129. doi: 10.1016/j.mayocp.2021.09.005.
PMID: 34863399
4. Urinary incontinence and pelvic organ prolapse in women: management NICE
guideline Published:2April2019, www.nice.org.uk/guidance/ng123
5. International urogynecology consultation chapter 3 committee 2; conservative
treatment of patient with pelvic organ prolapse: Pelvic floor muscle training. Kari
Bø , Sònia Anglès-Acedo, Achla Batra , Ingeborg Hoff Brækken , Yi Ling Chan ,
Cristine Homsi Jorge , Jennifer Kruger , Manisha Yadav , Chantale Dumoulin
11 Ottobre 2022
6. Li C, Gong Y, Wang B. The efficacy of pelvic floor muscle training for pelvic
organ prolapse: a systematic review and meta-analysis. Int Urogynecol J. 2016
Jul;27(7):981-92. doi: 10.1007/s00192-015-2846-y. Epub 2015 Sep 25. PMID:
26407564.
7. American Urogynecologic Society Best Practice Statement:Evaluation and
Counseling of Patients With Pelvic Organ Prolapse. Copyright © 2017 Wolters
Kluwer Health | Lippincott Williams & Wilkins. Unauthorized reproduction of this
article is prohibited
8. Evaluation and Management of Pelvic Organ Prolapse, Rubin Raju, MD, and Brian
J. Linder, MD Mayo Clin Proc. n December 2021;96(12):3122-3129 n
https://doi.org/10.1016/j.mayocp.2021.09.005
9. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic
organ prolapse. Adi Y. Weintraub 1, Hannah Glinter 1, Naama Marcus-Braun 2. 1
Department of Obstetrics and Gynecology, Soroka University Medical Center,
Faculty of Medicine, Ben-Gurion University of the Negev, Beer-Sheba, Israel; 2
75
Department of Obstetrics and Gynecology, ZivMedical Center, Faculty of
Medicine, Bar-Ilan university, Safed, Israel
10. Family history and pelvic organ prolapse: a systematic review and meta-analysis
Parisa Samimi1 & Sarah H. Jones2 & Ayush Giri2,3 Received: 10 July 2020
/Accepted: 2 October 2020; The International Urogynecological Association 2020
11. Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al.
Prevalence and trends of symptomatic pelvic floor disorders in U.S. women.
Obstet Gynecol. 2014;123:141-8.
12. Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current
observations and future projections. Am J Obstet Gynecol. 2001 Jun;184(7):1496-
501; discussion 1501-3. doi: 10.1067/mob.2001.114868. PMID: 11408873..
13. Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated
systematic review and meta-analysis Sascha F. M. Schulten, MD; Marieke J. Claas-
Quax, MD, PhD; Mirjam Weemhoff, MD, PhD; Hugo W. van Eijndhoven, MD,
PhD; Sanne A. van Leijsen, MD, PhD; Tineke F. Vergeldt, MD, PhD; Joanna
IntHout, PhD; Kirsten B. Kluivers, MD, PhD Systematic Review, AUGUST 2022
American Journal of Obstetrics & Gynecology
14. Hallock JL, Handa VL. The Epidemiology of Pelvic Floor Disorders and
Childbirth: An Update. Obstet Gynecol Clin North Am. 2016 Mar;43(1):1-13. doi:
10.1016/j.ogc.2015.10.008. PMID: 26880504; PMCID: PMC4757815.
15. Veit-Rubin N, Cartwright R, Singh AU, Digesu GA, Fernando R, Khullar V.
Association between joint hypermobility and pelvic organ prolapse in women: a
systematic review and meta-analysis. Int Urogynecol J. 2016;27:1469-78.
16. Patel DA, Xu X, Thomason AD, Ransom SB, Ivy JS, DeLancey JO. Childbirth and
pelvic floor dysfunction: an epidemiologic approach to the assessment of
prevention opportunities at delivery. Am J Obstet Gynecol.2006;195:23-8.
17. Volløyhaug I, Mørkved S, Salvesen Ø, Salvesen KÅ. Forceps delivery is associated
with increased risk of pelvic organ prolapse and muscle trauma: a cross-sectional
study 16-24 years after first delivery. Ultrasound Obstet Gynecol 2015;46:487–95.
18. Glazener C, Elders A, MacArthur C, et al.Childbirth and prolapse: long-term
associations with the symptoms andobjectivemeasurement of pelvic organ prolapse.
BJOG 2013;120:161–8.
76
19. Petros PE, Woodman PJ. The Integral Theory of continence. Int Urogynecol J
Pelvic Floor Dysfunct. 2008 Jan;19(1):35-40. doi: 10.1007/s00192-007-0475-9.
Epub 2007 Oct 30. PMID: 17968480.
20. Swift S, Woodman P, O’Boyle A, et al. Pelvic Organ Support Study (POSST): the
distribution, clinical definition, and epidemiologic condition of pelvic organ
support defects. Am J Obstet Gynecol 2005;192(3): 795–806. Bradley CS, Nygaard
IE. Vaginal wall descensus and pelvic floor symptoms in older women. Obstet
Gynecol 2005;106(4):759–766.
21. American Urogynecologic Society Best Practice Statement: Evaluation and
Counseling of Patients With Pelvic Organ Prolapse. Female Pelvic Med Reconstr
Surg. 2017 Sep/Oct;23(5):281-287. doi: 10.1097/SPV.0000000000000424. Erratum
in: Female Pelvic Med Reconstr Surg. 2018 May/Jun;24(3):256. PMID: 28846554.
22. MeisterMR, Sutcliffe S,Ghetti C, et al. Development of a standardized,
reproducible screening examination for assessment of pelvic floor myofascial pain.
Am J Obstet Gynecol. 2019;220(3):255.e1-e9.
23. Pelvic organ prolapse: ACOG Practice Bulletin, Number 214. Obstet Gynecol.
2019;134(5):e126-e142. Chen CCG, Cox JT, Yuan C, Thomaier L, Dutta S.
Knowledge of pelvic floor disorders in women seeking primary care: a cross-
sectional study. BMC Fam Pract. 2019;20(1):70.
24. MeisterMR, Sutcliffe S,Ghetti C, et al. Development of a standardized,reproducible
screening examination for assessment of pelvic floor myofascial pain. Am J Obstet
Gynecol. 2019;220(3):255.e1-e9.
25. Urinary incontinence and pelvic organ prolapse in women: management
NICE guideline Published: 2 April 2019, www.nice.org.uk/guidance/ng123
26. Bo K, Frawley HC, Haylen BT, et al. An International Urogynecological
Association (IUGA)/International Continence Society (ICS) joint report on the
terminology for the conservative and nonpharmacological management of female
pelvic floor dysfunction. Neurourol Urodyn. 2017;36(2) 221‐244.
https://doi.org/10.1002/nau.23107)
27. (Hagen S, Stark D. Conservative prevention and management of pelvic organ
prolapse in women. Cochrane Database Syst Rev. 2011;(12)):003882.
https://doi.org/10.1002/14651858.CD003882.
77
28. Completeness of exercise reporting among randomized controlled trials on pelvic
floor muscle training for women with pelvic organ prolapse: A systematic review
Silvia Giagio Tiziano Innocenti, Stefano Salvioli, Alessandra Lami, Maria Cristina
Meriggiola, Paolo Pillastrini1, Giulia Gava.
29. Impact of pelvic floor muscle training in pelvic organ prolapse Ritu Basnet1
Received: 26 July 2020 /Accepted: 11 November 2020 # The International
Urogynecological Association 2021. https://doi.org/10.1007/s00192-021-04875-y
30. Effects of Pelvic-Floor Muscle Training in Patients with Pelvic Organ Prolapse
Approached with Surgery vs. Conservative Treatment: A Systematic Review.
Andrea Espiño-Albela 1, Carla Castaño-García 2, Esther Díaz-Mohedo 3,* and
Alfonso Javier Ibáñez-Vera
31. (Are hypopressive and other exercise programs effective for the treatment of pelvic
organ prolapse? Kari Bø1,2 · Sònia Angles‑Acedo3 · Achla Batra4 · Ingeborg H.
Brækken5,6 · Yi Ling Chan7 · Cristine Homsi Jorge8 · Jennifer Kruger9 · Manisha
Yadav10 · Chantale Dumoulin. https://doi.org/10.1007/s00192-022-05407-y
32. Martín-Rodríguez S, Bo K. Is abdominal hypopressive technique effective in the
prevention and treatment of pelvic floor dysfunction? Marketing or evidence from
high-quality clinical trials? Br J Sports Med. 2019;53(2):135–6. https:// doi. org/
10. 1136/ bjsports- 2017- 098046.
33. Hernández RRV. Efficacy of hypopressive abdominal gymnastics in rehabilitating
the pelvic floor of women: a systematic review. Actas, Urol Esp (Engl Ed).
2018;42(9):557–66. https:// doi. org/ 10. 1016/j. acuro. 2017. 10. 004.)
34. Resende APM, Bernardes BT, Stupp L, Oliveira E, Castro RA, Girao M, Sartori
MGF. Pelvic floor muscle training is better than hypopressive exercises in pelvic
organ prolapse treatment: an assessor-blinded randomized controlled trial.
Neurourol Urodyn. 2019;38(1):171–9. https:// doi. org/ 10. 1002/ nau. 23819.
35. Navarro-Brazález B, Prieto-Gómez V, Prieto-Merino D, Sánchez-Sánchez B,
McLean L, Torres-Lacomba M. Effectiveness of hypopressive exercises in women
with pelvic floor dysfunction: a randomised controlled trial. J Clin Med.
2020;9(4):1149. https:// doi. org/10. 3390/ jcm90 41149.
36. Reman T, Cacciari L, Voelkl JG, Malcolm D, Budgett D, Kruger J,Dumoulin C.
Intravaginal pressure profile during two diaphragmatic aspiration tasks in women
with stress urinary incontinence: a cross sectional study. Neurourol Urodyn.
2020;39(S2).
78
37. Mowat A, Maher D, Baessler K, Christmann-Schmid C, Haya N, Maher C. Surgery
for women with posterior compartment prolapse. Cochrane Database Syst Rev.
2018 Mar 5;3(3):CD012975. doi: 10.1002/14651858.CD012975. PMID: 29502352;
PMCID: PMC6494287.
38. Alas AN, Bresee C, Eilber K, et al. Measuring the quality of care provided to
women with pelvic organ prolapse. Am J Obstet Gynecol 2015;212(4):471.e1–
471.e9. doi:10.1016/j.ajog.2014.10.1105.
39. Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for
managing pelvic organ prolapse in women. Cochrane Database Syst Rev
2020;11:CD004010. doi:10.1002/14651858. CD004010.pub4.
40. Urogynecology (Phila) . 2023 Jan 1;29(1):5-20. doi:
10.1097/SPV.0000000000001293. Vaginal Pessary Use and Management for
Pelvic Organ Prolapse: Developed by the joint writing group of the American
Urogynecologic Society and the Society of Urologic Nurses and Associates.
Individual writing group members are noted in the Acknowledgments section . No
authors listed PMID: 36548101 DOI: 10.1097/SPV.0000000000001293
41. UK Clinical Guideline for best practice in the use of vaginal pessaries for pelvic
organ prolapse
42. (Efficacy of biofeedback on quality of life in stages I and II pelvic organ prolapse:
A Pilot study. Tannaz Ahadi, Neda Taghvadoost, Soheila Aminimoghaddam, Bijan
Forogh, Roxana Bazazbehbahani, Gholam Reza Raissi.
Published:June 15, 2017 DOI:https://doi.org/10.1016/j.ejogrb.2017.06.023
43. Evaluation of the effect of electrical stimulation combined with biofeedback
therapy for postpartum pelvic organ prolapse: a static and dynamic magnetic
resonance imaging study. Wang Qiujing , Zhao Yujiao , Huang Lixiang , Zhang
Jing , Shen Wen , Authors Info & Affiliations. Published: 2019 -01 -29 ·DOI:
10.3760/cma.j.issn.0376-2491.2019.05.011
44. Electrical stimulation plus biofeedback improves urination function, pelvic floor
function, and distress after reconstructive surgery:a randomized controlled trial.
Aiming Lv1 · Tianzi Gai 1 · Sichen Zhang1 · Qing Feng1 · Ye Li.
Vol.:(0123456789)1 3International Journal of Colorectal Disease (2023) 38:226
https://doi.org/10.1007/s00384-023-04513-7
45. Original Article Clinical effect of electrical stimulation biofeedback therapy
combined with pelvic floor functional exercise on postpartum pelvic organ prolapse
79
CVFulian Zhong, Wenbin Miao, Zhixia Yu, Lu Hong, Ni’na Deng. PMID:
34306406 PMCID: PMC8290786
46. Berghmans B, Seleme. The ‘5 F’s concept for pelvic floor muscle training: from
finding the pelvic floor to functional use. J Womens Health. 2020;3:131–4.
47. Deffieux X, Hubeaux K, Porcher R, Sheikh Ismael S, Raibaut P, Amarenco G.
Abnormal pelvic response to cough in women With stress urinary incontinence.
Neurourol Urodyn. 2008;27(4):291–6. https://doi.org/10.1002/nau.20506.
48. Bø MS. Pelvic floor and exercise science. In: Bø K, Berghmans MS, Van Kampen
M, editors. Evidence-based physical therapyfor the pelvic floor bridging science
and clinical practice. 2nd ed. Edinburgh: Elsevier; 2015. p. 111–6.
49. Impact of pelvic floor muscle training in pelvic organ prolapse Ritu Basnet1
Received: 26 July 2020 /Accepted: 11 November 2020. The International
Urogynecological Association 2021, International Urogynecology Journal,
https://doi.org/10.1007/s00192-020-04613-w)
50. Effects of Pelvic-Floor Muscle Training in Patients with Pelvic Organ Prolapse
Approached with Surgery vs. Conservative Treatment: A Systematic Review.
Andrea Espiño-Albela , Carla Castaño-García , Esther Díaz-Mohedo and Alfonso
Javier Ibáñez-Vera
51. “Is PREHAB in Pelvic Floor Surgery Needed? A Topical Review Jacek K.
Szymański, Małgorzata Starzec‐Proserpio, Aneta Słabuszewska‐Jóźwiak and
Grzegorz Jakiel
52. Bø, K. Pelvic floor muscle training in treatment of female stress urinary
incontinence, pelvic organ prolapse and sexual dysfunction. World J. Urol. 2012,
30, 437–443.
Snowden, C.P.; Anderson, H. Preoperative optimization: Rationale and process: Is
it economic sense? Curr.Opin. Anaesthesiol. 2012, 25, 210–216