Marinari Noemi [University of Florence, Florence, Italy]
Ferrarello Francesco [Unit of Functional Rehabilitation, Department of Allied Health Professions, Azienda USL Toscana Centro, Prato, Italy.
Serafini Isabella [University of Florence, Florence, Italy]
Effective communication between health care professionals (HCPs) and patients is recognized as being a fundamental clinical skill. Research has found that effective communication leads to significant benefits such as patient satisfaction, resolution of symptoms, improved functioning, and better psychological status.
An overview of systematic reviews on training strategies for teaching communication skills was published by Berkhof et al.1 They concluded that role-play, feedback, and small group discussions are effective training strategies.
Our purpose was to identify effective methods for teaching communication skills to HCPs in order to facilitate communication in hospitals, nursing homes and health care institutions. In particular, we were interested in understanding how successful teaching was in changing the communicative behavior of health care workers, and how significantly this might affect their work.
Study design: overview of systematic reviews.
Data resources: MedLine, PsycINFO and EMBASE. Last data search, 31 December 2023.
Eligibility criteria: systematic reviews or meta-analyses published in English language from march 2009 (last data search of Berkhof et al.1). To be included, studies had to involve licensed HCPs, communication with adult patients, and communication training programs for HCPs.
We extracted data on the characteristics of the studies included in the reviews. Specifically we investigated study design, sample size, target population, participants’ professional profile, interventions researched (e.g., educational strategies, delivery modality, setting, duration), and outcome measures.
We systematically assessed the methodological quality of the included studies with the AMSTAR-2 tool.
We synthesized the findings through qualitative analysis.
We retrieved eight systematic reviews on communication skills training programs for HCPs, including 2-17 studies (mean, 9.75).2-9 The participants were physicians, nurses, midwives, and physiotherapists. One study focused on feedback, while most reported on mixed-strategy approaches. Components of the interventions were lectures (7 reviews), role-playing (6 reviews), feedback (5 reviews), active review session (3 reviews), and clinical cases discussion (2 reviews).
Out of 21 outcome measures, the most used were self-efficacy (5 reviews) and communication skills (3 reviews).
Some evidence for the effectiveness of using training courses to improve HCPs’ communication skills exists. Moore et al., in their Cochrane review, found that a variety of communication skills training courses are likely to improve HCPs’ empathy.3
According to the AMSTAR-2 tool the reviews ranged in levels of confidence from low (4 studies) to critically low (4 studies).
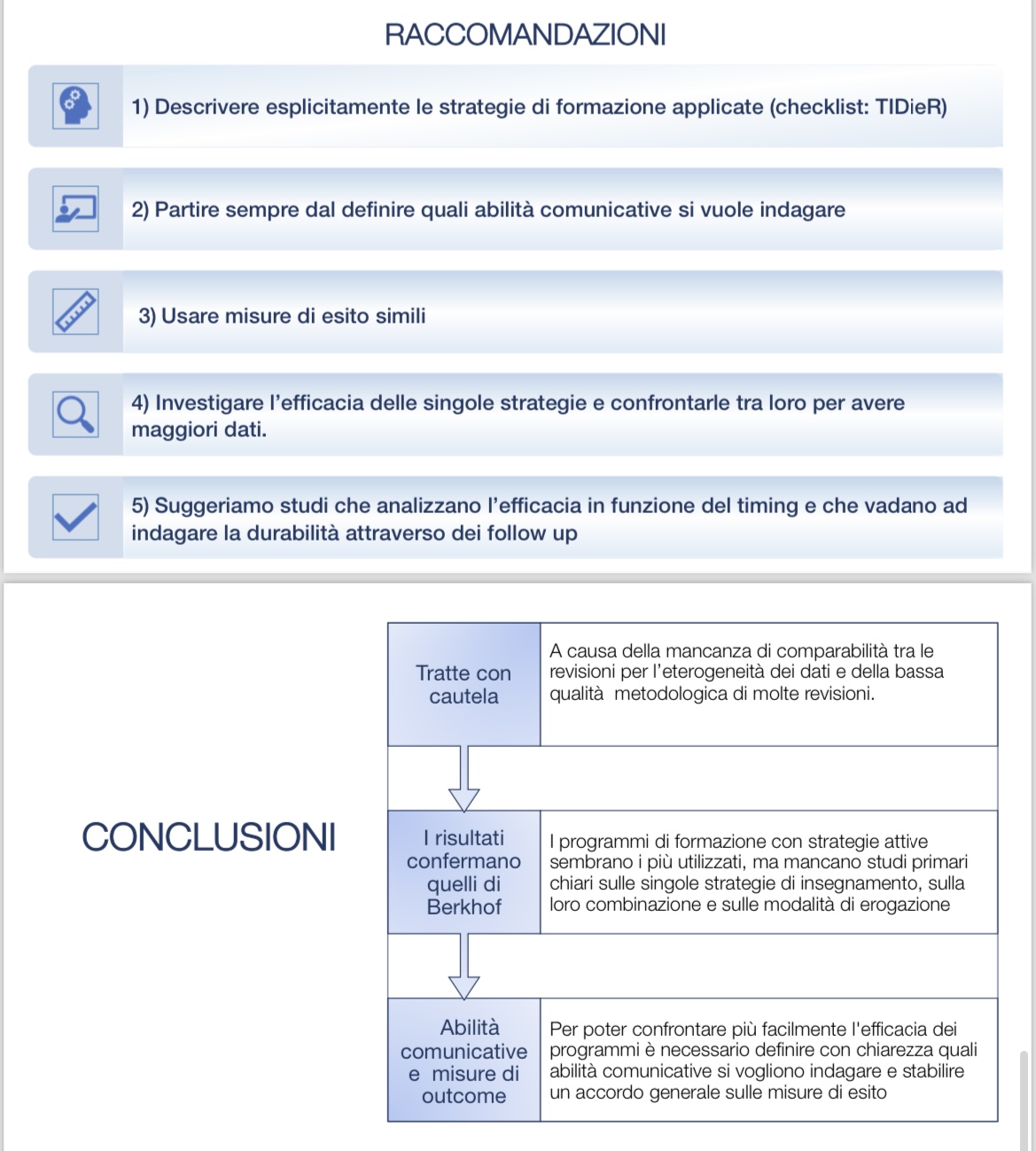
Although the reviews included studies on role-playing, feedback, and small group discussions, interventions reported as effective by Berkhof et al.,1 no new evidence have emerged on strategies for teaching communication skills. In particular, there is no clear evidence of which modality (e.g., intensive), duration, or combination of training strategies is the most effective in a learning program.
There is a lack of primary studies on each of the teaching strategies, their combinations, and delivery methods. Such studies could help to understand which educational strategy is the most effective for teaching communication skills to HCPs. The results of our overview confirm the conclusions of Berkhof et al., on the need to establish general agreement on outcome measures in order to compare the effectiveness of training programs.1