Feller Daniel (Department of General Practice, Erasmus MC, University Medical Centre, Rotterdam, The Netherlands)
Wingbermuhle Roel (Department of General Practice, Erasmus MC, University Medical Centre, Rotterdam, The Netherlands)
Berg Bjørnar (Centre for Intelligent Musculoskeletal Health, Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway)
Nesse Vigdal Ørjan (Centre for Intelligent Musculoskeletal Health, Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway)
Innocenti Tiziano (Department of Health Sciences, Faculty of Science, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences, The Netherlands)
Grotle Margreth (Centre for Intelligent Musculoskeletal Health, Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway)
Ostelo Raymond (Department of Health Sciences, Faculty of Science, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences, The Netherlands)
Chiarotto Alessandro (Department of General Practice, Erasmus MC, University Medical Centre, Rotterdam, The Netherlands)
Clinicians can use prediction models to inform decision-making, such as determining the best course of treatment for a patient based on their prognosis. 1 However, this can be achieved only if the development or validation study is described in sufficient detail to enable the clinician to use the model. 1 Also, accurate reporting of the models’ development or validation is crucial to allowing other researchers to assess their validity and reliability, reproduce or replicate the study, or build upon the findings in future research. 1 Currently, no studies have assessed the completeness of the reporting in studies that develop or validate a (prognostic or diagnostic) prediction model for patients with spinal pain or osteoarthritis (OA). Therefore, the objective of this study was to evaluate the completeness of reporting of prediction model studies in patients with spinal pain or OA in terms of adherence to the “Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis” (TRIPOD). 1
We searched for prognostic and diagnostic prediction models in patients with spinal pain or OA in MEDLINE, Embase, Web of Science, and CINHAL. We limited our search from January 2016 to the 17th of March 2023. We used this time framework because the TRIPOD checklist was published in 2015, and we assumed some delay from publication and potential widespread use. Reference lists of the included studies and bibliographic information of relevant systematic reviews were also checked. Using a standardized adherence assessment form published by Heus et al. 2, we assessed the adherence to the TRIPOD statement of the included studies. Two pairs of independent reviewers performed the study selection and data extraction phases.
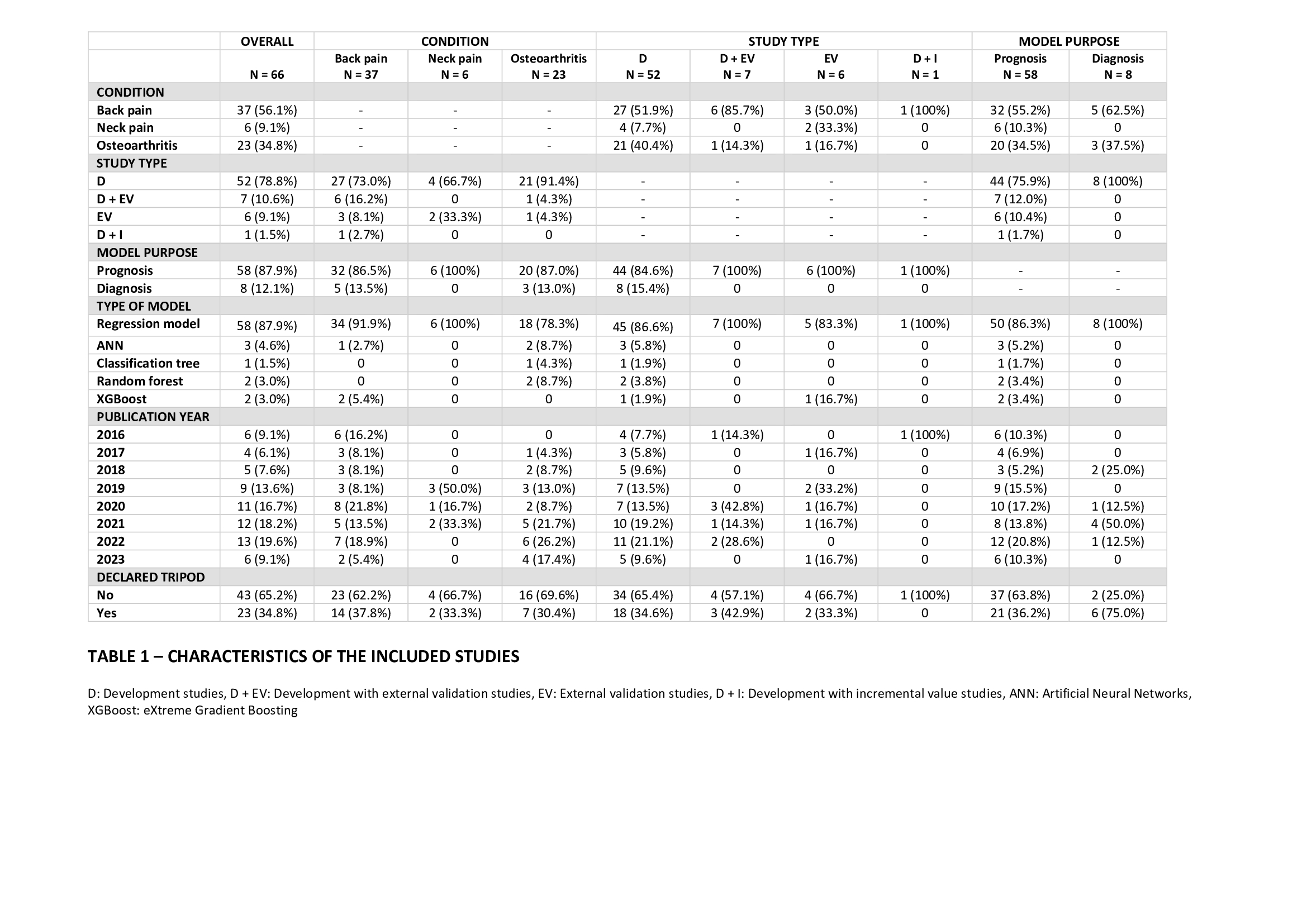
We included 66 studies. The majority of the studies (56.1%) focused on back pain. Most studies (80.3%) developed a model without external validation and 87.9% focused on prognostic models. Of all the studies, 87.9% used regression-based models, while the remaining 12.1% employed machine learning techniques. Most of the studies (65.2%) did not declare to have used the TRIPOD statement (Table 1).
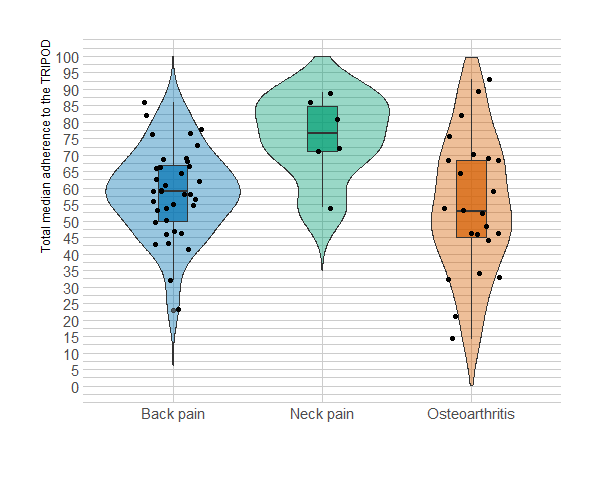
The median adherence to the TRIPOD was 59% overall (IQR: 21.8) (Figure 1). The difference in the median adherence between studies that declared the use of the TRIPOD and those that did not was 4%. Furthermore, we did not observe any improvement in adherence over the years. The items in the methods and results sections were the ones with the worst reporting, while the items in the discussion and background were the ones with the best reporting. Notably, only 42.2% of the studies fully described participant characteristics, just 10% reported model-building procedures and internal validation methods, and less than half of the studies reported performance measures (i.e., discrimination and calibration).
The adherence to the TRIPOD of prediction models in the spinal pain and OA field is limited. Due to the reporting below desirable standards, clinicians may encounter difficulties in effectively applying a model in clinical practice, and researchers cannot judge the model’s validity or build on research findings. Thus, future studies on prediction models in spinal pain and OA should follow the TRIPOD statement for their reporting. The use of the TRIPOD should be encouraged by peer reviewers and journal editors, for example, by mentioning the TRIPOD as the mandatory reporting guideline for prediction model studies in the “instruction for authors” section of the journal. 2 Journals and editors should also adopt stricter strategies to check for reporting completeness 3, and the biomedical literature, in general, should increase authors’ awareness about the importance of complete reporting, as it is probably one of the barriers to fully implementing the reporting guidelines and why there has been no improvement in adherence over the years. 4