Malaspina Vissia [Ast Fermo, Italia]
Bragagnolo Matteo [Ast Fermo, Italia]
Grasso Anna Maria [Ast Fermo, Italia]
Ependymomas are rare glial tumors with clinical and biological heterogeneity, categorized into supratentorial ependymoma, posterior fossa ependymoma, and spinal cord ependymoma, depending on anatomical localization.(1).
Treatment involves primarily surgical resection, aiming at maximal safe resection: the extent of resection is the most important prognostic factor.(2)
The main symptoms are sensory and motor deficit, hyposthenia, coordination and balance deficit, and Bladder or bowel dysfunction. (3)
Post-surgical rehabilitation can improve the consequences of surgery and maintain a good quality of life, especially in young patients with long life expectancy. (4)
With this case report, we describe the results obtained from rehabilitation treatment aimed at improving sphincters control and sexual dysfunctions after C1 -C3 intramedullary ependymoma removal surgery by laminectomy.
The patient is a 45-year-old nulliparous woman who underwent laminectomy surgery for removal of cervical ependymoma. She takes Lirica 150 mg 1×2/day and pregabalin 350 mg/day.
At T0 the patient had left hemilateral paresthesia, also involving the saddle area, vulvar, intra vulvar and anal areas; severe hypo-pallesthesia at AAIIs going back to SIAS. She left AI sthenic deficits (F3).
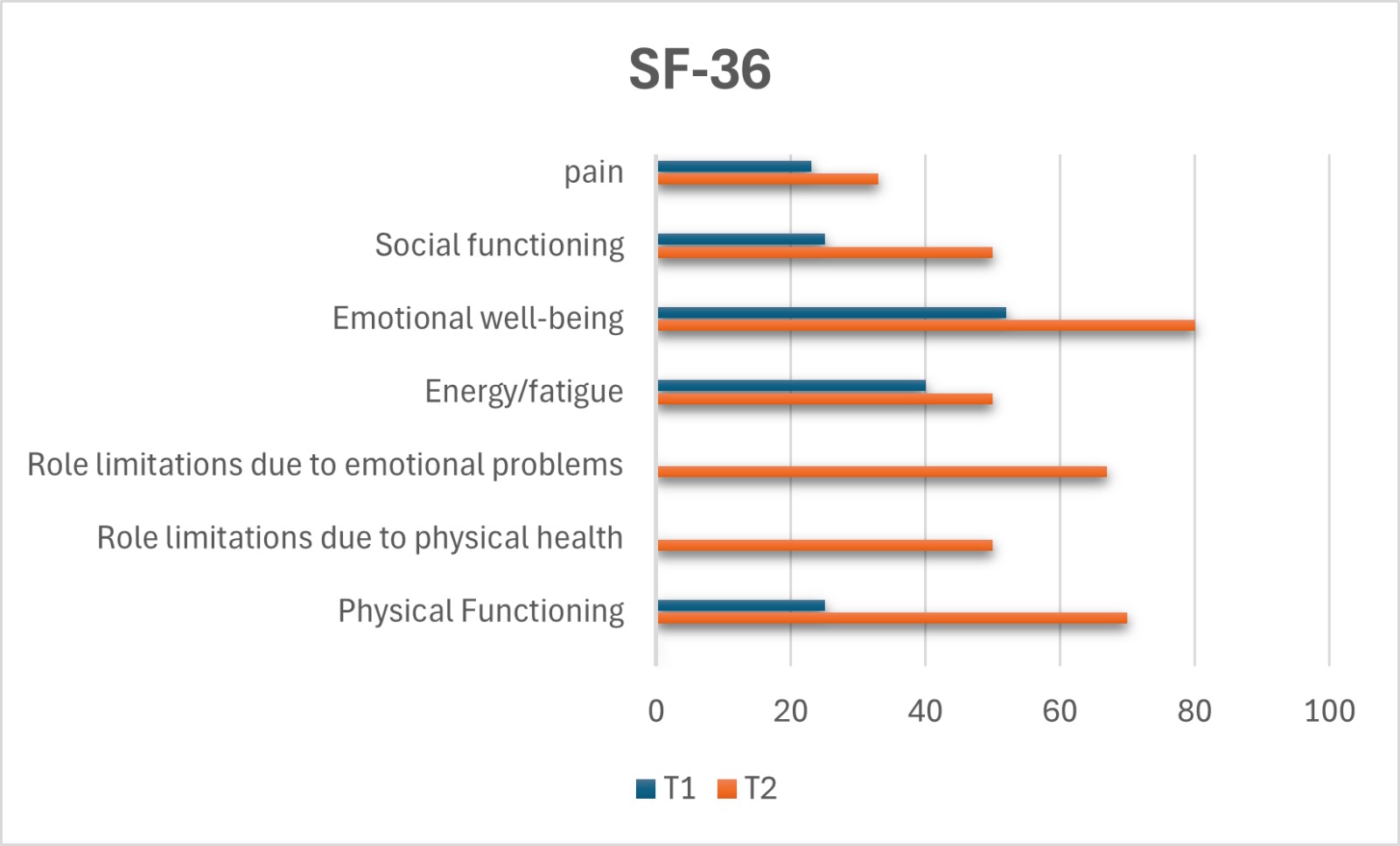
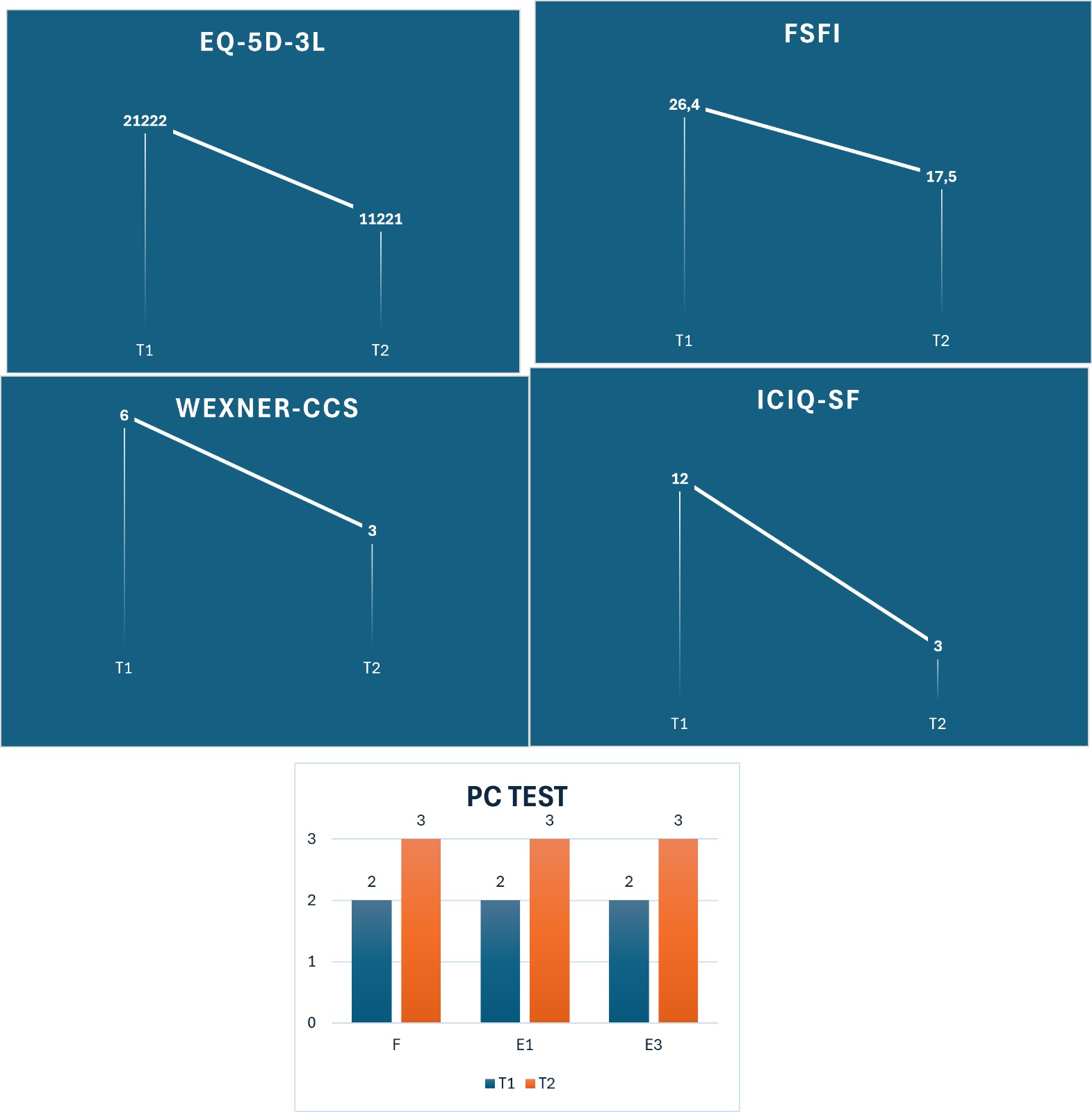
Perineal sensitivity, pelvic floor muscle (PC test), urinary and fecal leakage (ICIQ-SF and WEXNER-CCS), quality of daily living (SF-36 and EQ-5D-3L), and sexual function (FSFI) were assessed at first and last session.
The treatment lasted 4 months (two days a week for 2 months and once a week for another 2 months, not during menstruation).
Manual techniques were adopted to release trigger points, in association with pelvic floor muscle exercises, also through the use of BFB, and sensory discrimination (tactile, pressure and thermal) and proprioceptive exercises in the perineal area.
All parameters assessed at evaluation (T0) improved at the end of treatment (T1).
Sensitivity and proprioception in the perineal area improved. There was an increase in pelvic floor muscle function (PC Test T0: F2, E1-2, E2-2; T1; F3, E1-3, E2-3) with a reduction in urinary incontinence (ICIQ-SF T0: 12/21; T1 3/21) and fecal incontinence (WEXNER-CCS T0: 6/20; T1: 3/20), leading to an improvement in quality of life [SF 36 T0: physical functioning 25/100, role limitations due to physical health 0/100, role limitations due to emotional problems 0/100, energy 40/100, emotional well-being 52/100, social functioning 25/100, pain 23/100, general health 45/100; T1: physical functioning 70/100, role limitations due to physical health 50/100, role limitations due to emotional problems 67/100, energy 50/100, emotional well-being 80/100, social functioning 50/100, pain 33/100, general health 50/100. EQ-5D-3L T0: 21222 (0.377), T1 11221 (0.679)] and sexual functions (FSFI T0: 26.4; T1; 17.5).
Physiotherapy treatment through functional exercise of the pelvic muscles, also with the support of biofeedback, and proprioceptive exercises with devices of different surfaces and consistencies, has led to an increase in sensitivity in the pelvic area, an increase in pelvic motor control and to a reduction in urinary and fecal incontinence. The main factor to focus on was improving quality of life and sexual function. There are still few studies in the literature that evaluate the effectiveness of the rehabilitation treatment of perineal dysfunction on patients with incomplete spinal cord injury. Future work could investigate this further and include follow-ups to verify the maintenance of the results obtained.
(1) Cerretti, G., Pessina, F., Franceschi, E., Barresi, V., Salvalaggio, A., Padovan, M., Manara, R., di Nunno, V., Bono, B. C., Librizzi, G., Caccese, M., Scorsetti, M., Maccari, M., Minniti, G., Navarria, P., & Lombardi, G. (2023). Spinal ependymoma in adults: from molecular advances to new treatment perspectives. In Frontiers in Oncology (Vol. 13). Frontiers Media SA. https://doi.org/10.3389/fonc.2023.1301179
(2) Weber DC, Wang Y, Miller R, et al. Long-term outcome of patients with spinal myxopapillary ependymoma: treatment results from the MD Anderson Cancer Center and institutions from the Rare Cancer Network. Neuro Oncol. 2015;17(4):588–95.
(3) Abdulaziz M, Mallory GW, Bydon M, et al. Outcomes following myxopapillary ependymoma resection: the importance of capsule integrity. Neurosurg Focus. 2015;39(2):E8.
(4)Suzuki, T., Tsuji, O., Ichikawa, M., Ishii, R., Nagoshi, N., Kawakami, M., Watanabe, K., Matsumoto, M., Tsuji, T., Fujiwara, T., & Nakamura, M. (2023). Early Phase Functional Recovery after Spinal Intramedullary Tumor Resection Could Predict Ambulatory Capacity at 1 Year after Surgery. Asian Spine Journal, 17(2), 355–364. https://doi.org/10.31616/asj.2022.0068