Baldo Niccolò (Azienda ospedaliero-universitaria Senese – Strada delle Scotte, 14, 53100 – Siena (SI) – Italy)
Disability rates are increasing worldwide (1, 2, 3) and the main aim of rehabilitation is to maximize functionality despite disability, impacting the quality of life of individuals and caregivers (1, 4). The extension of life causes an increase in hospitalizations in the Medical Area and, since these are mostly frail elderly people, therefore with increased vulnerability and limited functional reserve, stress factors such as hospitalization can also worsen any disability already present (5, 6). These characteristics determine the need to activate early physiotherapy management in the acute phase of hospitalization and highlight the need to optimize the use of the increasingly limited personnel resources present.
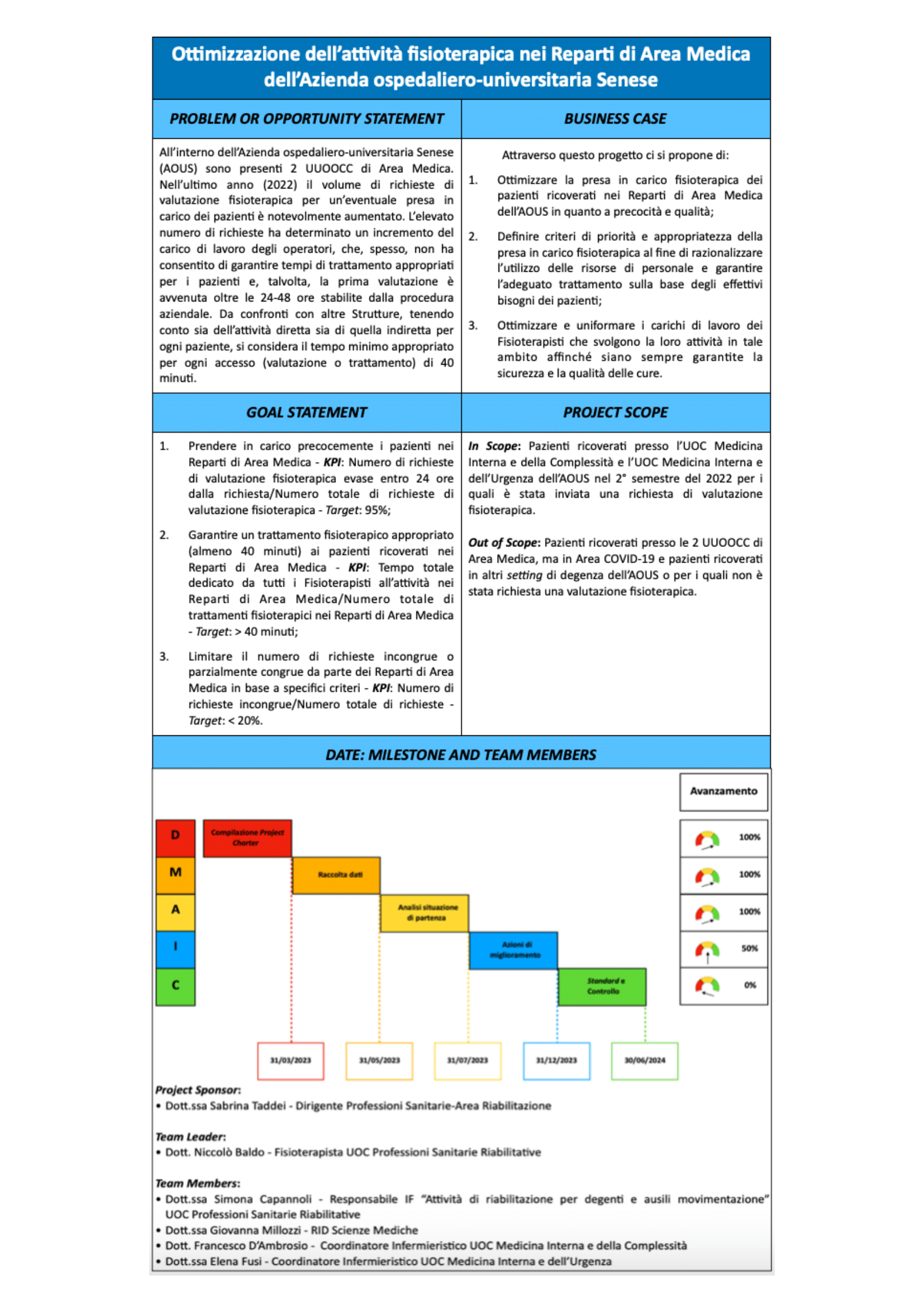
The objectives of this work were the optimization of the care of patients hospitalized in the Medical Area of the Azienda ospedaliero-universitaria Senese, the definition of priority and appropriateness criteria and the optimization and standardization of Physiotherapists’ workloads. To carry out the project, the logical path set on the phases defined by the Six Sigma’s acronym DMAIC was followed (DEFINE: Problem’s identification through the creation of a Project Charter that defines and plans the entire project; MEASURE: Measurement and collection of data, focusing attention on the type of patients, characteristics of the inpatient Departments, organization of the Rehabilitation Health Professions Unit and activities of the Physiotherapist staff at the Medical Area in question; ANALYZE: Interpretation of data and analysis of the root causes of the problem; IMPROVE: Generation and implementation of corrective actions; CONTROL: Monitoring and standardization of the optimized system).
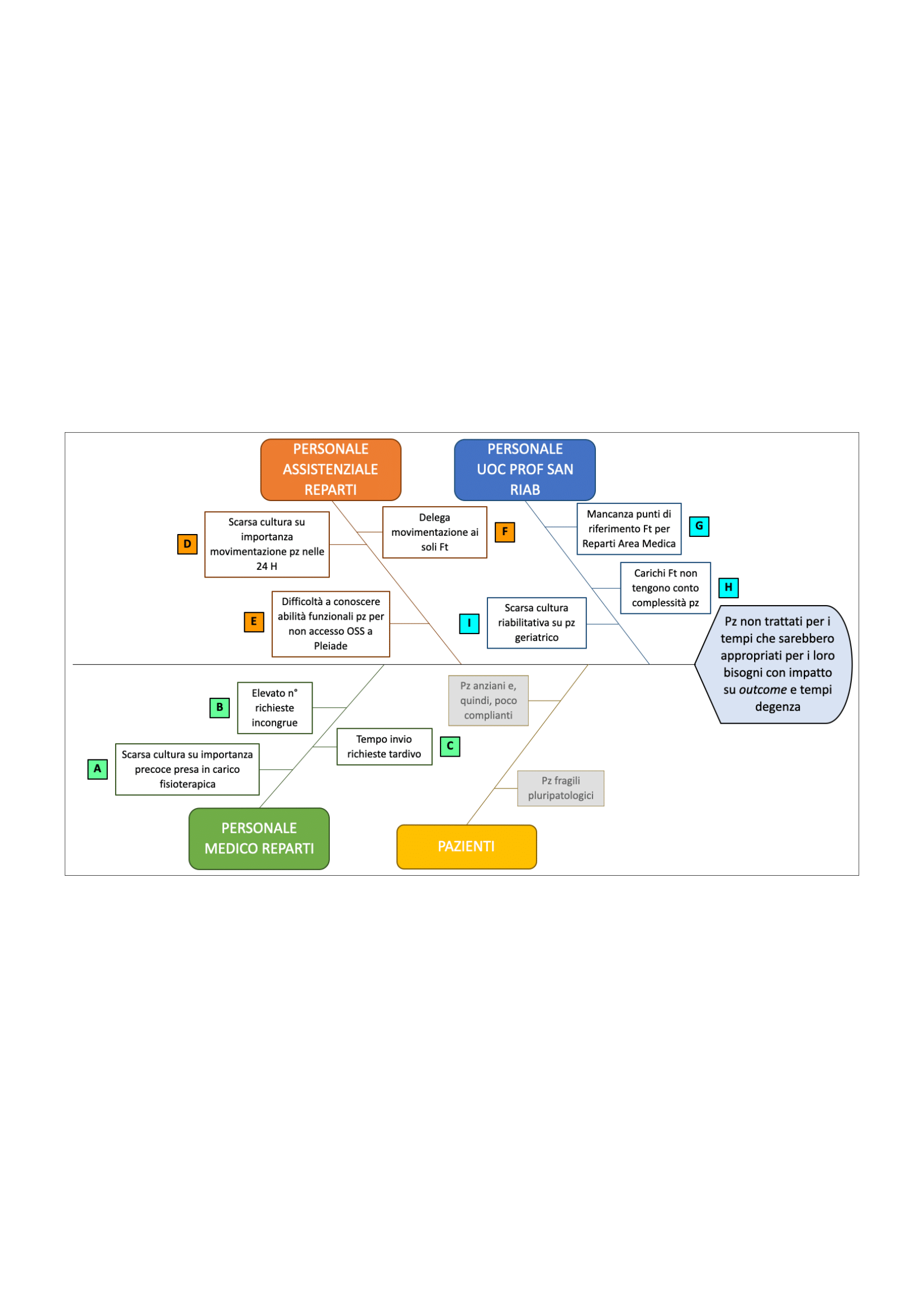
From the analysis of the measured data, critical issues emerged such as: 1) The time dedicated to the patient, considering direct and indirect activities, is lower than that defined by comparisons with other facilities, in the absence of shared standards, and compared to the needs and characteristics of the patients; 2) Some initial assessments carried out 4-5 days after the request due to the high volume of consultations activated; 3) A high percentage of assessments carried out in which treatment was not activated due to inconsistent requests; 4) Differences in the percentage of requests for evaluation on the total hospitalizations for pathology between the 2 Units of the Medical Area of the Azienda ospedaliero-universitaria Senese which denoted different rehabilitation culture.
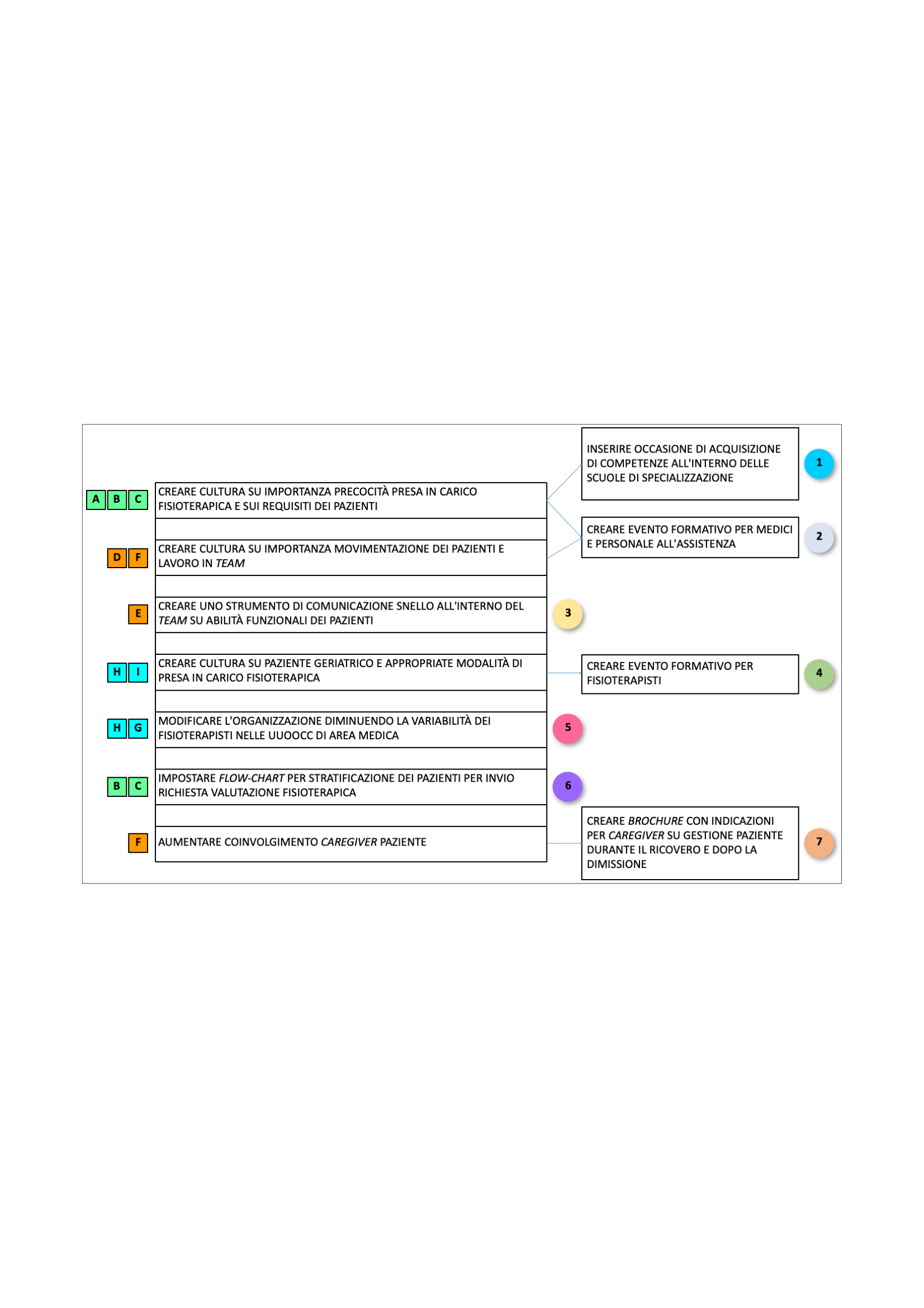
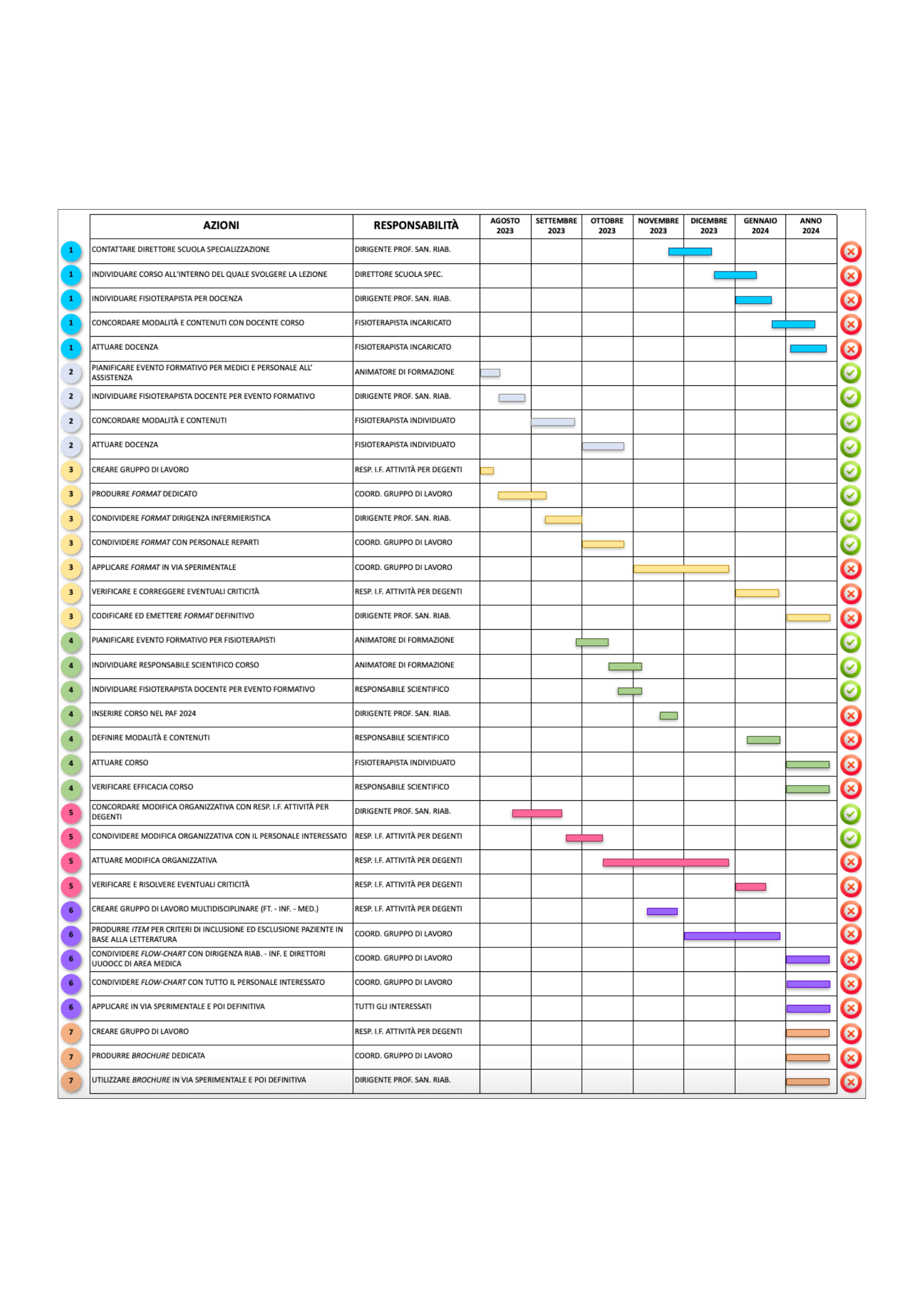
Starting from the analysis of the root causes, the countermeasures to be implemented were identified, the improvement actions were found and their implementation was designed and planned with the related times and responsibilities. The main ones were the creation of a culture on the importance of early physiotherapy management and patient handling, the setting up of a flow-chart for patient stratification and the definition of a shared communication tool on functional abilities. The expected advantages concerned both the users, since evaluating and treating the right patient in the right time and with the right modality provides a better quality of the intervention and better outcomes, and the organization, influencing hospitalization times and guaranteeing workloads for the Physiotherapists who allow you to work in quality and safety. Data collection is underway to verify the achievement of the set indicators.
1 Chan L, et al. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil 2002; 83:1196.
2 Vos T, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2163.
3 Murray CJ, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2197.
4 Gobbens RJ, et al. The predictive validity of the Tilburg Frailty Indicator: disability, health care utilization, and quality of life in a population at risk. Gerontologist 2012; 52:619.
5 Fried LP, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56:M146-56.
6 Rockwood K, et al. Frailty in Relation to the Accumulation of Deficits. J Gerontol A Biol Sci Med Sci 2007; 62:722-7.