Fu, Yanyan [Department of General Practice, Erasmus University Medical Center, Rotterdam, The Netherlands]
Feller, Daniel [Department of General Practice, Erasmus University Medical Center, Rotterdam, The Netherlands; Provincial Agency for Health of the Autonomous Province of Trento, Trento, Italy]
Koes, Bart [Department of General Practice, Erasmus University Medical Center, Rotterdam, The Netherlands; Research Unit of General Practice, Department of Public Health and the Center for Muscle and Joint Health, University of Southern Denmark, Odense, Denmark]
Chiarotto, Alessandro [Department of General Practice, Erasmus University Medical Center, Rotterdam, The Netherlands]
The prognosis for patients with non-specific low back pain (LBP) can be difficult to determine due to the wide variation in its trajectory. 2 Relying on single prognostic factors such as age, gender, and pain intensity alone is not accurate enough for predicting the prognosis of health conditions. 3 Therefore, it is recommended that clinicians use prognostic models, which are models designed to predict the prognosis of a health condition using a combination of patient socio-demographic characteristics, clinical variables, laboratory, and/or imaging data, to determine the progression of LBP better. 4 An example of a prognostic model in the LBP field is the STarT Back Screening Tool. 5 Currently, no reviews have been published focusing on prognostic models for chronic LBP. Therefore, our systematic review aims to summarize the available evidence on the risk of bias and predictive performance (i.e., discrimination and calibration) of prognostic models for chronic LBP.
This systematic review protocol was registered in PROSPERO. 6 We searched MEDLINE ALL, Embase, Web of Science Core Collection, and CINAHL databases from inception to July 13 2022, to retrieve observational cohort studies, nested case-control studies, and randomized controlled trials on the development or validation of prediction models for the prognosis of adult patients (≥18 years old) with chronic (duration > 3 months) non-specific LBP in primary care. Our outcomes of interest were physical functioning, pain intensity, and health-related quality of life at any follow-up time point. Data extraction was based on the “Checklist for critical Appraisal and data extraction for systematic Reviews of prediction Modelling Studies” (CHARMS), 7 while the risk of bias was judged using the “Prediction model Risk of Bias Assessment Tool” (PROBAST). 8 The study selection, data extraction and risk of bias assessment phases were performed by two authors independently. Due to the insufficient number of included studies and their clinical heterogeneity , we did not perform meta-analyses.
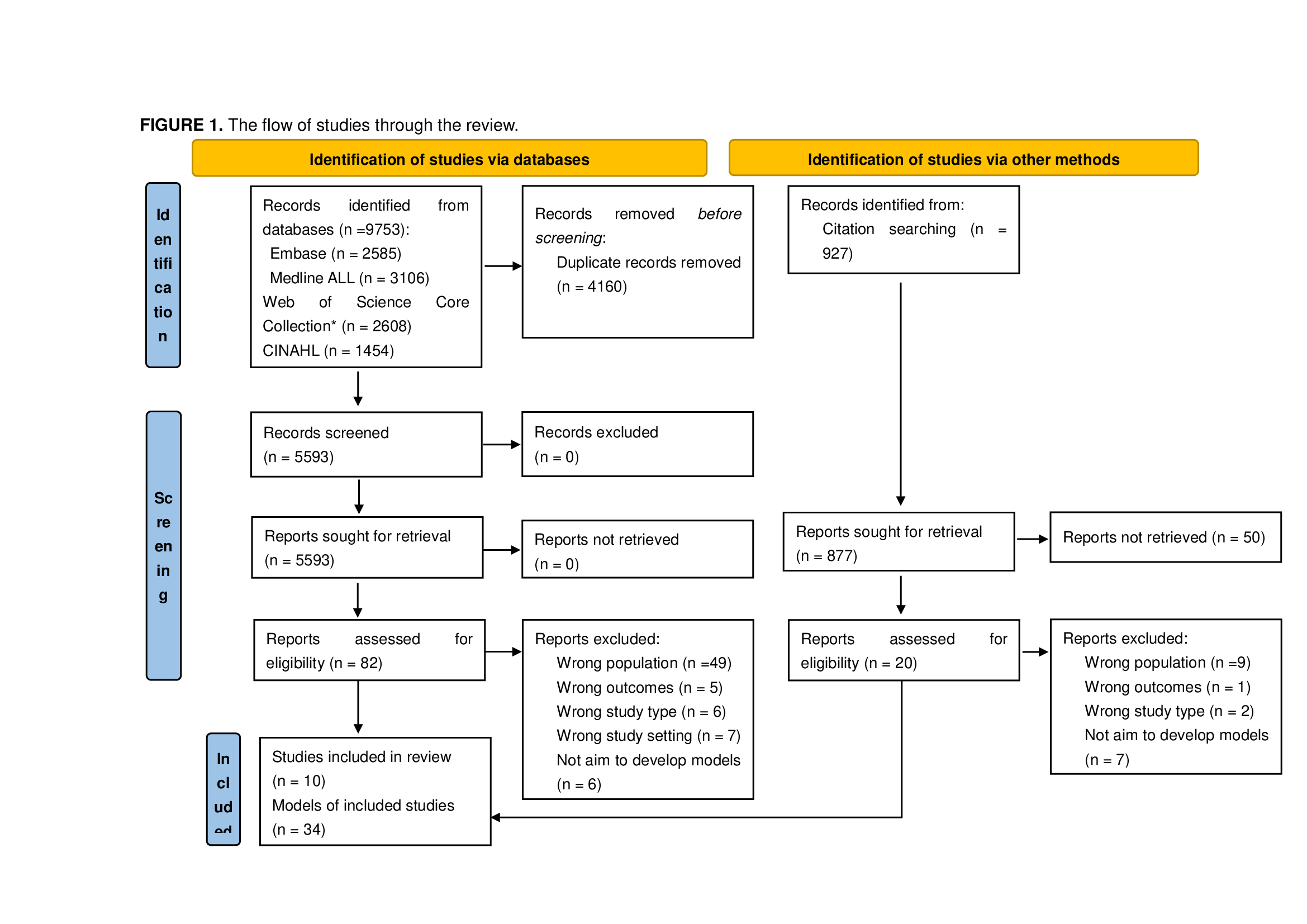
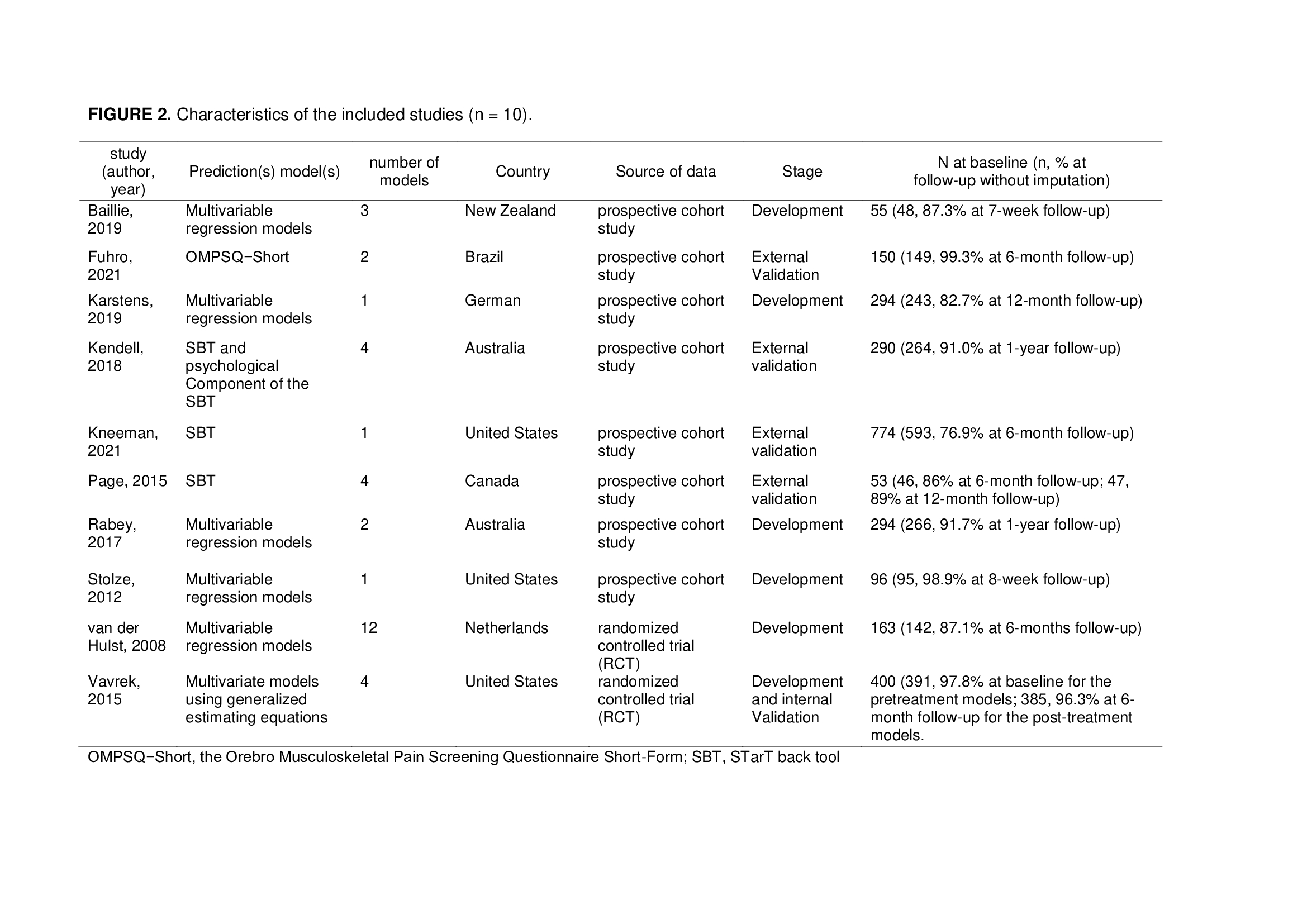
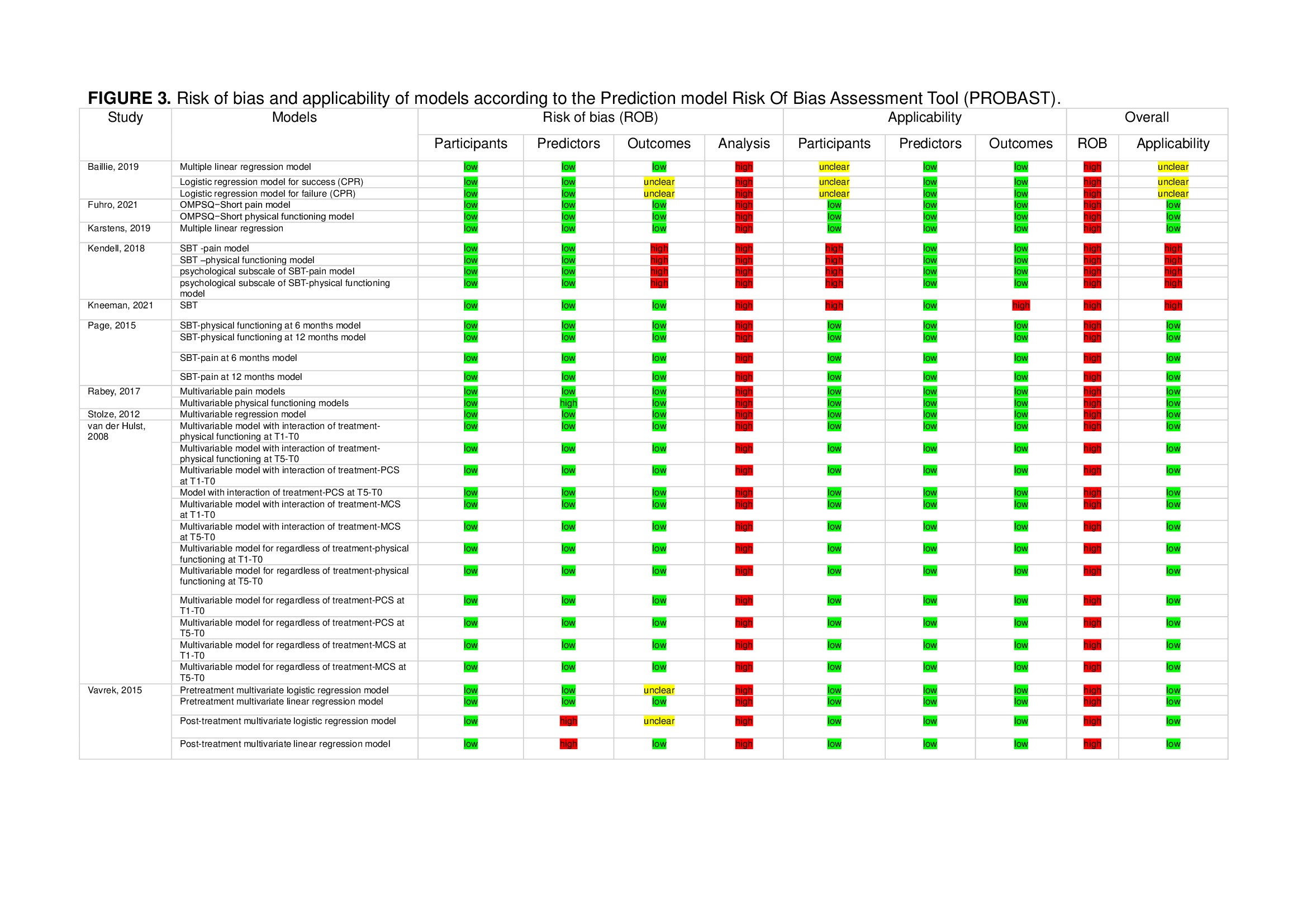
We included 10 studies including a total of 34 models (Figure 1). Of these, 19 were in the development stage, 11 were in the external validation stage, and 4 models were in the internal validation stage. The studies focused on evaluating the prognosis of LBP-related physical functioning (9 studies), pain intensity (5 studies), and health-related quality of life (1 study) (Figure 2). All models were found to have an overall high risk of bias due to a high bias in the analysis domain of the PROBAST (Figure 3), and none of the models reported calibration measures. The most promising models in terms of discrimination were the “Örebro Musculoskeletal Pain Screening Questionnaire – Short Form” (ÖMPSQ – Short) (1 external validation study; AUC 0.78, 95% CI 0.65 to 0.91) 9 and the STarT Back (3 external validation studies; AUC ranging from 0.71 to 0.84). 10–12
This systematic review is the first that aimed to search and evaluate all prognostic models for people with chronic LBP in primary care. All included models were found to have a high risk of bias (Figure 3). Additionally, due to inadequate reporting, it was not possible to fully assess the models’ performance in terms of both discrimination and calibration measures. The lack of reporting of calibration measures made it impossible to determine if the models accurately predicted the prognosis of LBP patients. Therefore, direct recommendations for the clinical use of existing models in predicting the prognosis of patients with chronic LBP cannot be provided. These results are consistent with systematic reviews of prognostic models for acute LBP, highlighting the need for more comprehensive research in this area. 13 Future studies on prognostic models for chronic LBP should focus on further external validation of the most promising models (ÖMPSQ – Short and the STarT Back), aiming to minimize bias with adequate reporting of all performance measures.