CARETTA INGRID – (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital – Reggio Emilia, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy.)
BENASSI MONICA – (Orthopedic Unit, Santa Maria Nuova Hospital – Reggio Emilia, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy)
MAZZOLA SONIA – (Orthopedic Unit, Santa Maria Nuova Hospital – Reggio Emilia, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy)
MANFREDI NICOLETTA – (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital – Reggio Emilia, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy.)
FIOCCHI ALENA – (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital – Reggio Emilia, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy)
RANCATI JACOPO MATTEO – (Care Management Unit, Azienda Unità Sanitaria Locale – IRCCS di Reggio Emilia – Italy)
Since the second half of 2020, our institution has introduced a pre-surgical planning model for rehabilitation pathways regarding patients scheduled for hip and knee replacement. The model involves profiling cases using the BRASS scale and a socio-environmental assessment. Profiling is carried out by the nurses of the Pre-Hospitalization Service and determines the discharge setting, whether inpatient or outpatient rehabilitation. The discharge destination is negotiated with the patients and recorded on specific electronic forms. The Pathway Manager Physiotherapist (FGP) monitors the surgical room schedule and pre-activates the networked rehabilitation services that will take over the cases after discharge. In the orthopedic ward, rehabilitation is initiated directly by physiotherapists, who, in collaboration with nursing and medical staff, inform the FGP of any need to reassess the pathway. In this study we report results about first 4 years of production.
During the first year of implementing the new model, a monitoring of several process indicators related to user adherence and pathway safety was developed by a specific database. This monitoring allowed to collect data relating to user participation and safety of pathway.
In the meanwhile of implementation we activated some adjustments to increase the timeliness and appropriateness of post-surgical interventions, including the activation of the medical staff in case of complications directly activated by the physiotherapist. Moreover, the workflows for sending outpatient cases (by FGP) were refined to improve rehabilitation continuity with direct access pathways, involving the rehabilitation team in case of emerging complexities, as reported by the physiotherapist.
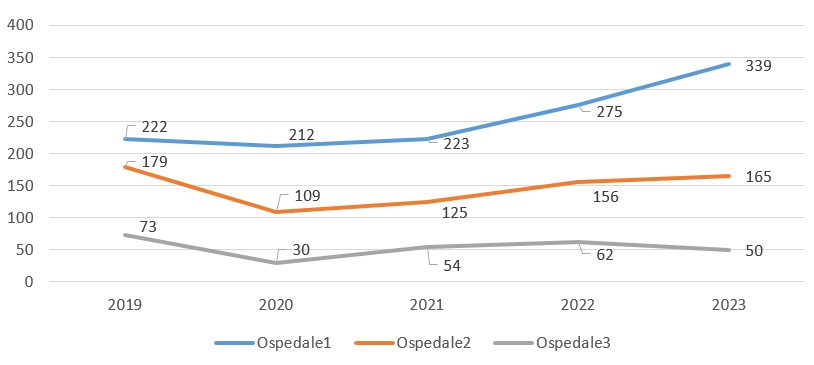
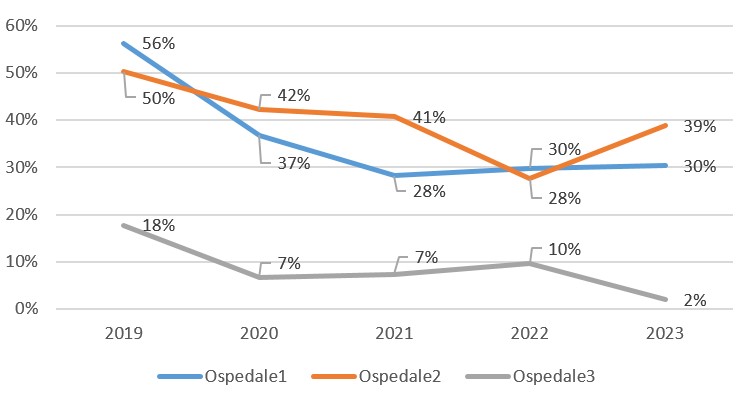
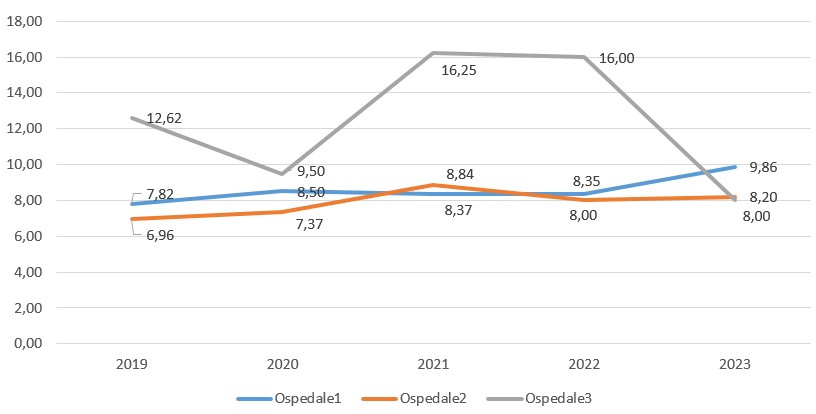
In the long term, the analysis was conducted based on the discharge form (SDO) flows on an annual basis, monitoring indicators related to average length of stay and the percentage of discharge to other care settings.
In the first year of implementation, 292 cases were profiled, and the user adherence rate to the proposed rehabilitation pathways was 88.7%. Factors that facilitated adherence to the outpatient pathway included the continuity of rehabilitation services offered and the fear of infectious risks associated with hospital stays (also due to the COVID-19 pandemic context). Obstacles included the absence of adequate family support and the presence of architectural barriers. No significant adverse events were recorded in the sample.
The need to revise planned pathways due to the emergence of complications affected 13 cases out of the 280 actually undergoing surgical intervention.
The SDO flows monitored annually from 2020 to 2023 highlighted a steady decline in cases managed in inpatient settings (from 50% to 30%), improving the appropriateness of settings, with no significant variations in the average length of stay (more detail in the attached images)
The implemented model highlights that rehabilitation pathway planning for the examined cases can be standardized and defined in the pre-surgical phase without compromising patient safety. The intervention of the medical staff is necessary if the predetermined pathway exhibits complications and can be directly activated by the physiotherapist within the rehabilitation team.
The model contributes to facilitating pathways in terms of intervention timeliness and rehabilitation continuity, concurrently improving appropriateness in the choice of care setting and resource utilization.
The role of a Pathway Manager Physiotherapist (FGP) is functional in governing patient flows within the service network in collaboration with other involved professionals. The model is potentially exportable and replicable; it requires the establishment of an interconnected network of rehabilitation services, a structured rehabilitation team, and can contribute to cost containment.