Messori Monica (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital, Reggio Emilia, Azienda USL-IRCCS di Reggio Emilia, Italy)
Fugazzaro Stefania (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital, Reggio Emilia, Azienda USL-IRCCS di Reggio Emilia, Italy)
Demola Andrea (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital, Reggio Emilia, Azienda USL-IRCCS di Reggio Emilia, Italy)
Manfredi Nicoletta (Physical Medicine and Rehabilitation Unit, Santa Maria Nuova Hospital, Reggio Emilia, Azienda USL-IRCCS di Reggio Emilia, Italy)
Brioni Tina (Physical Medicine and Rehabilitation Unit, Guastalla Civil Hospital, Azienda USL-IRCCS di Reggio Emilia, Italy)
Marotta Lucia (Physical Medicine and Rehabilitation Unit, Guastalla Civil Hospital, Azienda USL-IRCCS di Reggio Emilia, Italy)
Alessandri Alessandra (Physical Medicine and Rehabilitation Unit, Guastalla Civil Hospital, Azienda USL-IRCCS di Reggio Emilia, Italy)
Giberti Tiziana (Physical Medicine and Rehabilitation Unit, Sant’Anna Hospital, Castelnovo nè Monti, Azienda USL-IRCCS di Reggio Emilia, Italy)
Valeriani Samantha (Physical Medicine and Rehabilitation Unit, Sant’Anna Hospital, Castelnovo nè Monti, Azienda USL-IRCCS di Reggio Emilia, Italy)
Rancati Jacopo Matteo (Neuro-Motor and Rehabilitation Department– Direction of Health Professions, Azienda USL-IRCCS di Reggio Emilia, Italy)
Surgery represents the cornerstone of curative treatment for various types of cancer. However, surgery itself can have adverse effects on patient health. Enhanced Recovery After Surgery (ERAS) programs are patient-centered, multidisciplinary pathways developed to mitigate the surgical stress response, optimize physiological function, and facilitate recovery [1]. Multimodal prehabilitation involves multiple preoperative interventions aimed at preparing patients for surgery, enhancing resilience, and improving postoperative outcomes [2], [3]. Existing data on prehabilitation show considerable heterogeneity, particularly regarding adherence, which is crucial for ensuring program completion [4]. Given the brief preoperative timeframe, maintaining adherence is essential to maximize program effectiveness [5].
The aim of this study is to present the feasibility and patient adherence outcomes of the prehabilitation program implemented in our service.
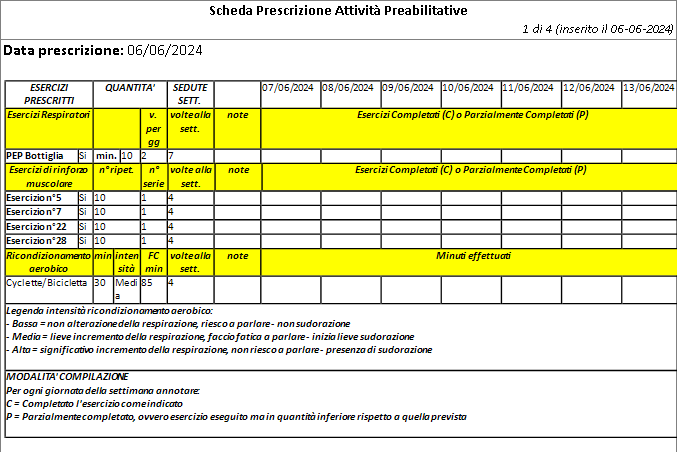
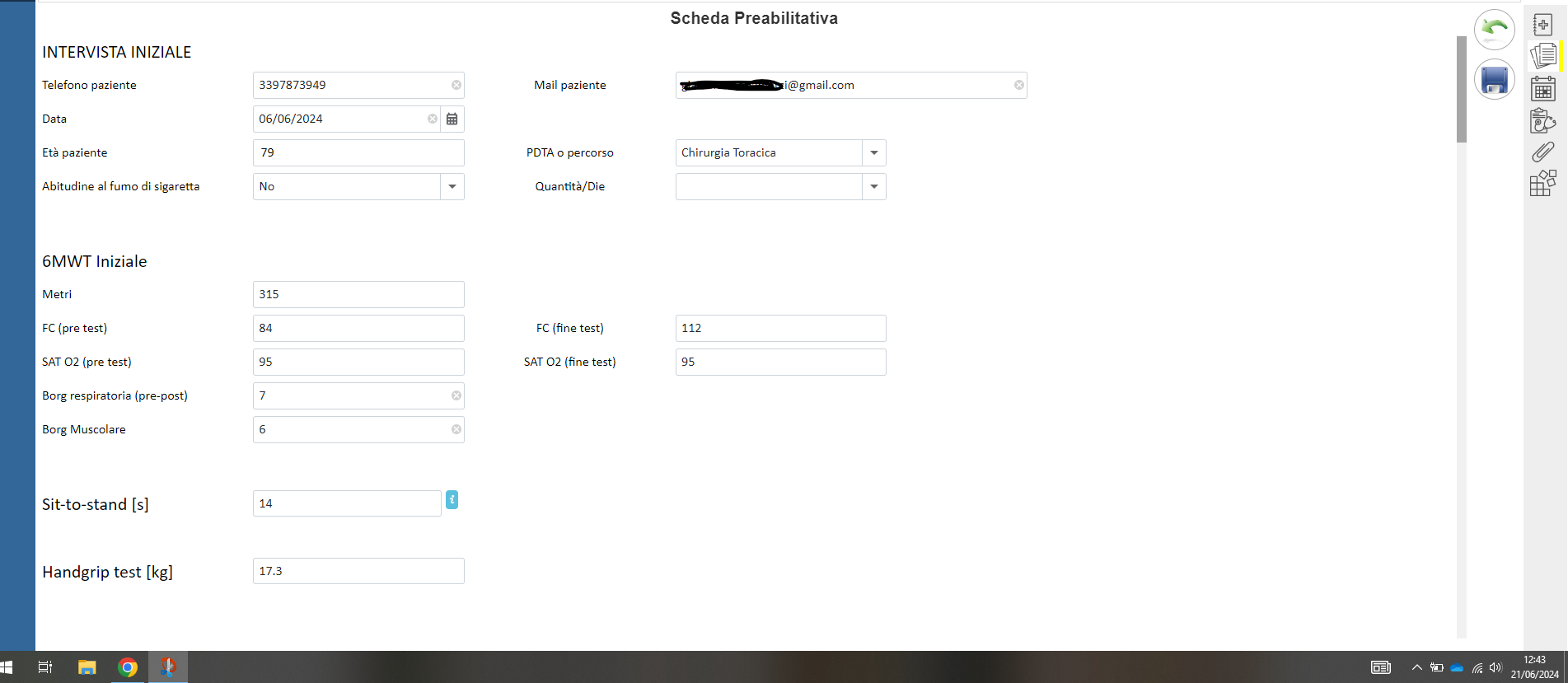
The prehabilitation program targets patients scheduled for thoracic and abdominal oncological surgery. To promote sustainability, enrollment criteria include: all candidates for thoracic surgery (due to the significant impact on functional ability) and candidates for abdominal surgery who meet at least three of the following criteria: age over 70 years, presence of cardiopulmonary diseases, expected surgery duration over 3 hours, and an “open” surgical approach. The initial session takes place at least 4 weeks prior to surgery. During this session, patients receive educational training and undergo an individual assessment to develop a tailored program, specifying the quantity, frequency, and intensity of exercises. The program includes respiratory exercises, muscle strengthening exercises and aerobic reconditioning. Patients receive a self-monitoring diary to track their adherence to the exercise regimen. A follow-up assessment is conducted the day before surgery.
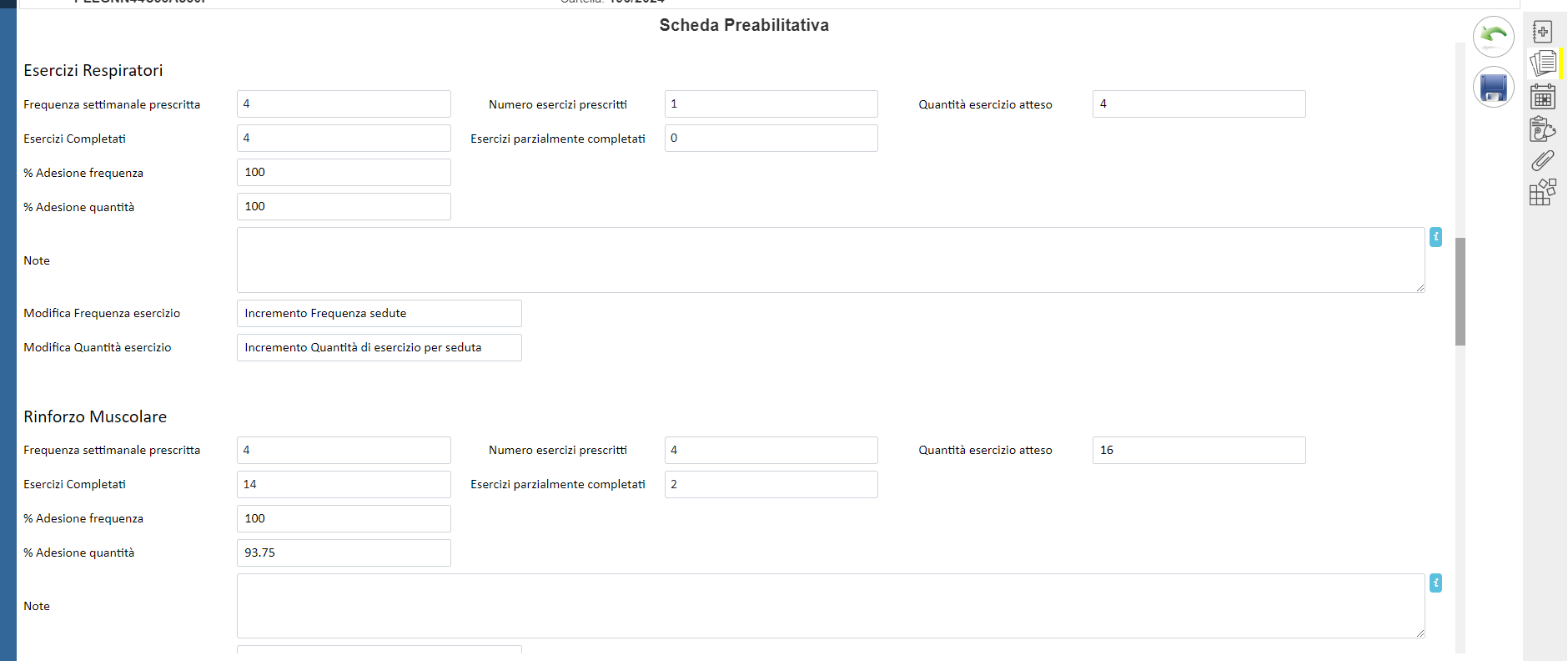
The program started at the beginning of June 2024, with the goal of reporting outcomes for 40 cases by November 2024. Clinical outcome indicators are being recorded, including the 6-minute walking test (6MWT), handgrip strength, sit-to-stand test, and patient adherence to the prescribed exercise regimen. The average duration of the prehabilitation program, targeted at 4 weeks, is also monitored. To design a highly personalized program, the physiotherapist collects detailed information on the type, frequency, duration, and intensity of the patient’s habitual physical activity during the initial interview. This information is documented in a dedicated electronic medical record. For the prescription of home exercises, the computerized system suggests the optimal progression based on the initial data, while the type of exercise is customized according to a standard protocol. The quantity and frequency of exercises performed, as recorded by the patient in a self-monitoring diary, are compared to the prescribed program to accurately calculate adherence.
With the implementation of this program, we aim to improve the cardiorespiratory and functional fitness of patients during the preoperative phase, thereby optimizing postoperative functional recovery and reducing the need for assistance. To achieve this, it is essential that patients adhere to the prescribed exercises and are referred to the program promptly, ensuring an exercise period of at least 3-4 weeks. Another critical factor for the success of this platform is the appropriateness of recruitment, focusing on enrolling the most deconditioned subjects who are at higher risk of postoperative respiratory complications and/or complications related to prolonged bed rest. In the long term, we consider it is useful to measure organizational outcomes such as the reduction in average length of hospital stay, readmission rates and the demand for healthcare services to manage postoperative complications.
[1] C. J. Molenaar, S. J. Van Rooijen, H. J. Fokkenrood, R. M. Roumen, L. Janssen, e G. D. Slooter, «Prehabilitation versus no prehabilitation to improve functional capacity, reduce postoperative complications and improve quality of life in colorectal cancer surgery», Cochrane Database of Systematic Reviews, vol. 2023, fasc. 6, mag. 2023, doi: 10.1002/14651858.CD013259.pub3.
[2] M. J. J. Voorn, E. J. M. Driessen, R. J. E. F. Reinders, V. E. M. Van Kampen-van Den Boogaart, B. C. Bongers, e M. L. G. Janssen-Heijnen, «Effects of exercise prehabilitation and/or rehabilitation on health-related quality of life and fatigue in patients with non-small cell lung cancer undergoing surgery: A systematic review», European Journal of Surgical Oncology, vol. 49, fasc. 10, p. 106909, ott. 2023, doi: 10.1016/j.ejso.2023.04.008.
[3] E. S. Bingül, N. M. Şentürk, e A. M. Kaynar, «Prehabilitation: a narrative review focused on exercise therapy for the prevention of postoperative pulmonary complications following lung resection», Front. Med., vol. 10, p. 1196981, ott. 2023, doi: 10.3389/fmed.2023.1196981.
[4] J. L. Waterland et al., «Prehabilitation in high-risk patients scheduled for major abdominal cancer surgery: a feasibility study», Perioper Med, vol. 11, fasc. 1, p. 32, ago. 2022, doi: 10.1186/s13741-022-00263-2.
[5] V. Ferreira et al., «Maximizing patient adherence to prehabilitation: what do the patients say?», Support Care Cancer, vol. 26, fasc. 8, pp. 2717–2723, ago. 2018, doi: 10.1007/s00520-018-4109-1.