Bò Maria Chiara [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]; Cavazzuti Lorenzo [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Bassi Maria Chiara [Medical Library, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Lusuardi Mirco [Neuromotor and Rehabilitation Department, Azienda USL-IRCCS Reggio Emilia, Correggio (Reggio Emilia), Italy]
Cavallieri Francesco [Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL-IRCCS di Reggio Emilia, Viale Risorgimento 80, 42123, Reggio Emilia, Italy]
Di Rauso Giulia [Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL-IRCCS di Reggio Emilia, Viale Risorgimento 80, 42123, Reggio Emilia, Italy]
Valzania Franco [Neurology Unit, Neuromotor & Rehabilitation Department, Azienda USL-IRCCS di Reggio Emilia, Viale Risorgimento 80, 42123, Reggio Emilia, Italy]
Damiano Benedetta [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Scaltriti Sara [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Merlo Andrea [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Campanini Isabella [LAM – Motion Analysis Laboratory, Neuromotor and Rehabilitation Department, San Sebastiano Hospital, Azienda USL-IRCCS di Reggio Emilia, Correggio (Reggio Emilia), Italy]
Patients with Parkinson’s disease (pwPD) or Parkinsonism usually complain of impaired balance and are two to three times more likely to fall than healthy adults [1]. This reduces patient autonomy from caregivers and negatively affects their quality of life [2]. Instrumental posturography has been suggested in the literature as a valuable technique to quantitively assess static balance in pwPD [3], being used in nearly 500 papers over the last 24 years. However, it suffers from some limitations, such as the absence of a defined “normal pattern”, the lack of protocol standardization, and the large number of parameters that can be computed [4]. This systematic review aims to critically appraise the use of static posturography in pwPD, including the clinical, technical, and methodological aspects, and identify gaps hindering its translation into the clinical routine.
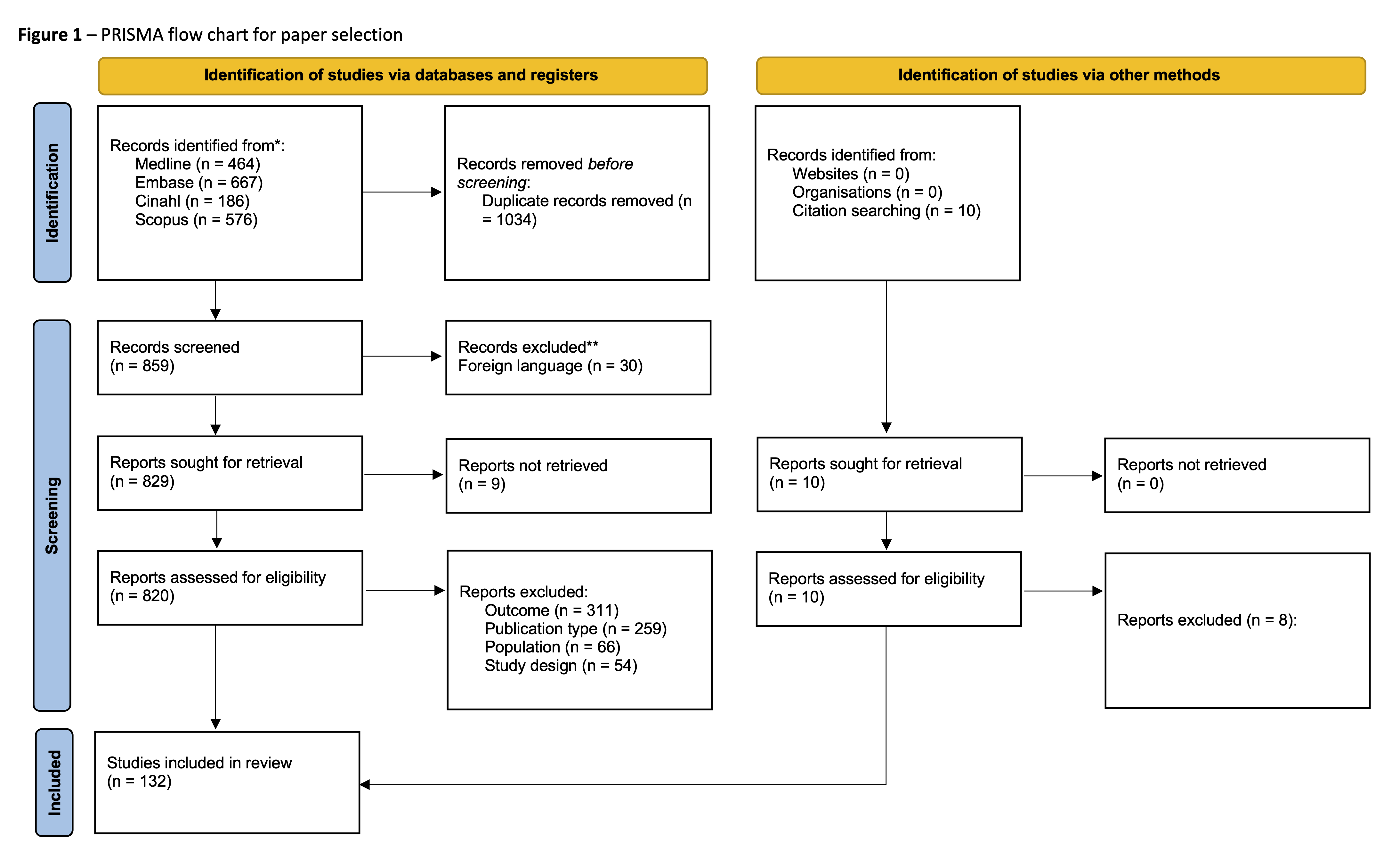
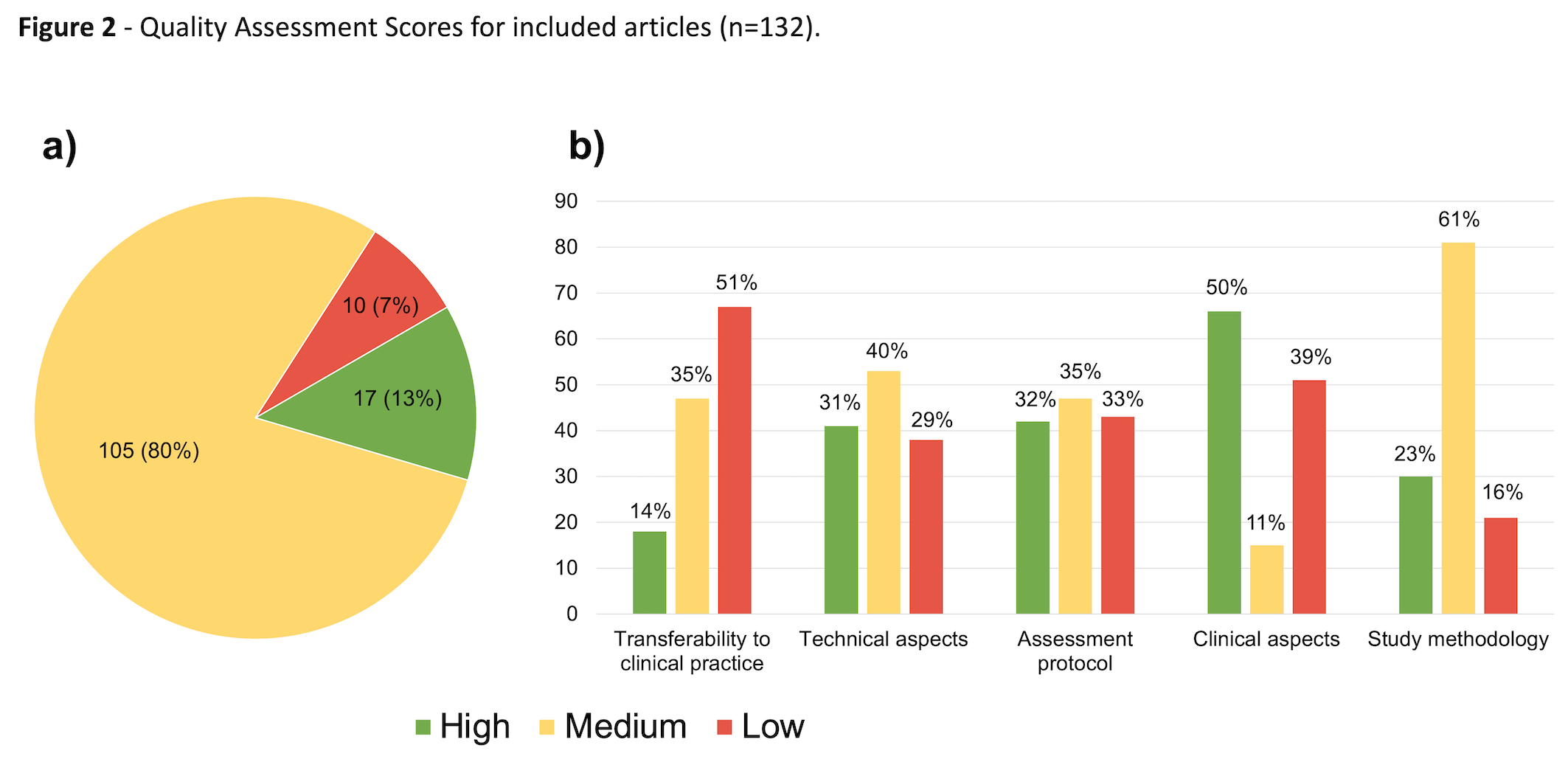
Four databases were searched for relevant articles by two blinded assessors. Primary studies on pwPD or Parkinsonism assessing the “baseline” condition (i.e., static posturography performed barefoot, in a bipedal upright stance, acquired with eyes open, on a firm surface) were included. A tailored set of 19 quality questions for the critical appraisal process was designed de novo, encompassing five different domains: study methodology, clinical aspects, assessment protocol, technical aspects, and transferability to clinical practice. Each question was scored on a three-level basis (i.e., 1 for “yes”, 0.5 for “limited details”, and 0 for “no”), plus a “not applicable” score. This allowed for the computation of domain-related and total percentage scores and the classification of studies as high-quality, medium-quality, and low-quality [5].
132 studies were included (Fig 1), involving 4262 pwPD. Most papers (105/132) were rated as medium-quality (Fig 2a). The domains with the lowest scores were “transferability to clinical practice” and “assessment protocol” (Fig 2b). The main flaw hindering translatability was the lack of a stated rationale behind the selection of specific protocols and posturographic parameters. From a clinical point of view, study samples lacked descriptive details and included patients with heterogeneous disease severity. Treatment techniques and dosages, when applicable, were overall well-detailed. From a methodological point of view, the lack of: 1) a-priori sample size design, 2) description of both the set-up and instructions given to the patients (e.g., foot and arm positioning, visual target), 3) relevant technical information (i.e., sampling frequency and filters), and 4) clarity on the formulas used to obtain parameters further limited the power of study results and protocol replicability.
Our customized critical appraisal highlighted several opportunities for enhancing the quality of studies on static posturography in the assessment of pwPD. In future studies, authors should: 1) discuss the rationale for choosing the assessment protocols and posturographic parameters to describe postural abilities of pwPD, 2) detail the inclusion criteria and select appropriate samples according to the aim of the study, and 3) report all the technical information to replicate the procedures and computations. Addressing these areas can significantly improve the external validity and clinical transferability of scientific literature to daily practice, which is key in biomedical research. This review provides useful references for each of the domains considered, supporting the rapid portability of findings to clinical settings.
[1] R.M. Pickering, Y.A.M. Grimbergen, U. Rigney, A. Ashburn, G. Mazibrada, B. Wood, P. Gray, G. Kerr, B.R. Bloem, A meta-analysis of six prospective studies of falling in Parkinson’s disease, Movement Disorders 22 (2007) 1892–1900. https://doi.org/10.1002/mds.21598.
[2] M. Michałowska, U. Fiszer, A. Krygowska-Wajs, K. Owczarek, Falls in Parkinson’s disease. Causes and impact on patients’ quality of life., Funct Neurol 20 (2005) 163–8. http://www.ncbi.nlm.nih.gov/pubmed/16483454.
[3] A. Kamieniarz, J. Michalska, A. Brachman, M. Pawłowski, K.J. Słomka, G. Juras, A posturographic procedure assessing balance disorders in parkinson’s disease: A systematic review, Clin Interv Aging 13 (2018) 2301–2316. https://doi.org/10.2147/CIA.S180894.
[4] L. Chiari, Stabilometry, in: Encyclopedia of Neuroscience, Springer Berlin Heidelberg, Berlin, Heidelberg, 2009: pp. 3830–3833. https://doi.org/10.1007/978-3-540-29678-2_5623.
[5] F. Samadi Kohnehshahri, A. Merlo, D. Mazzoli, M.C. Bò, R. Stagni, Machine learning applied to gait analysis data in cerebral palsy and stroke: A systematic review, Gait Posture 111 (2024) 105–121. https://doi.org/10.1016/j.gaitpost.2024.04.007.