Caratteristiche qualitative della Vulvodinia: Uno studio trasversale sui patterns di dolore genitale femminile
Qualitative Characteristics of Vulvodynia: A Cross-Sectional Study on Women’s Vulvar Pain Patterns
Introduction
Vulvodynia is a condition characterized by chronic pain in vulvar region, with a significant impact on women’s quality of life. [1] Its etiology remains poorly understood, and diagnosis is often challenging, relying on the exclusion of other specific causes of genital pain (e.g. infectious, neoplastic, neurological, etc.). [2] The identification of vulvodynia based on type of pain and symptomatic characteristics is crucial for appropriate clinical management. Previous studies have primarily focused on quantitative aspects of pain, but research on its qualitative characteristics is underexplored. This study aims to address this gap by examining the qualitative features of pain experienced by women with diagnosed vulvodynia using a body chart.
Methods
Following the STROBE guidelines , we conducted an observational cross-sectional study to analyze the qualitative pain characteristics in a population of women with a diagnosis of vulvodynia. Between December 2021 and May 2022, 82 women were recruited from patients attending FISIOS Pelvic-Perineal Disorders Rehabilitation Clinic. Among them, 72 participants met the inclusion criteria (according to the 2015 consensus of ISSVD, ISSWSH, and IPPS) [2] and were informed about the study’s nature before providing written informed and privacy consent forms.
Each participant completed a questionnaire to investigate intensity of pain using the Numeric Pain Rating Scale (NPRS) and associated symptoms. A pain drawing scale was utilized to explore the pain’s qualitative aspects.
Results
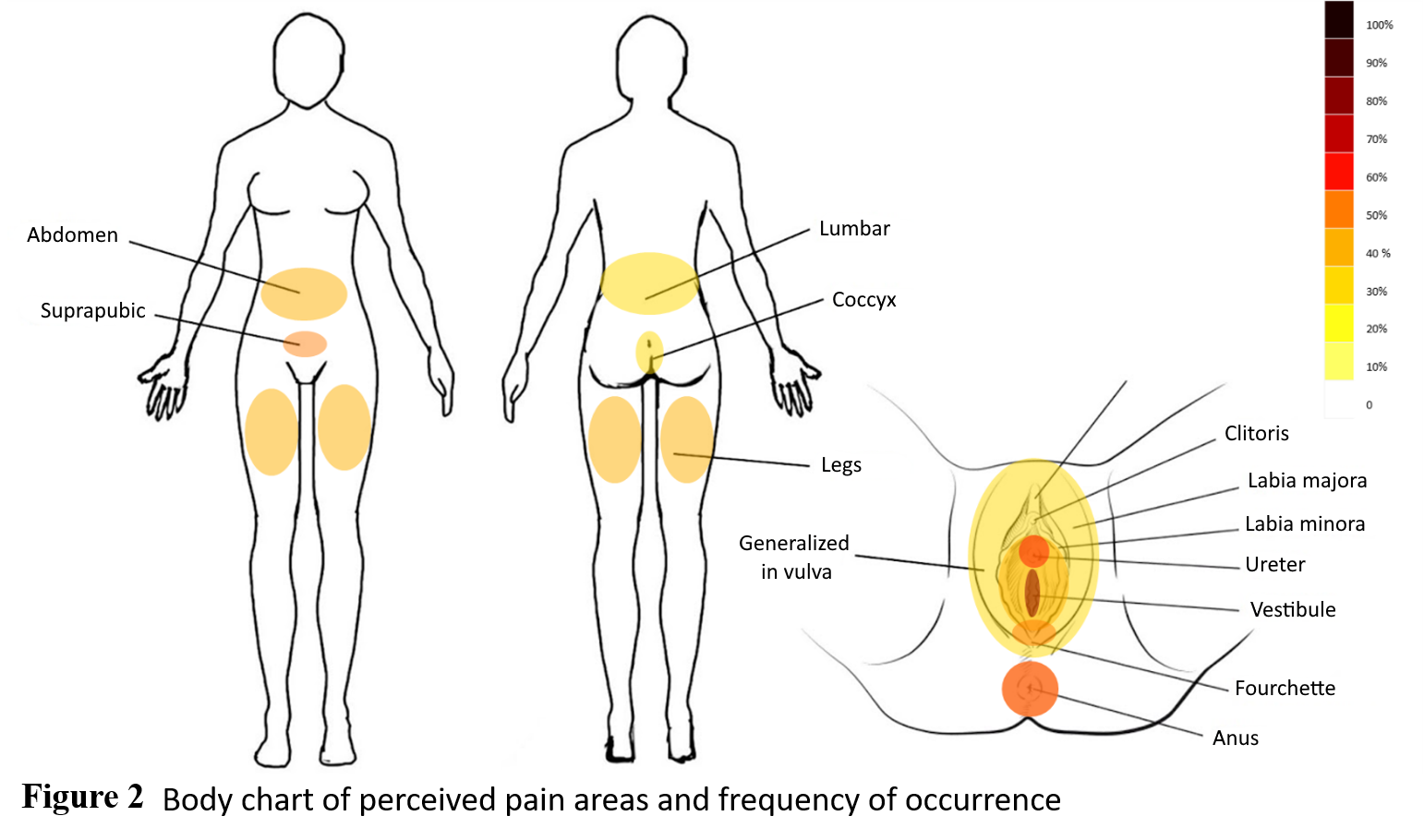
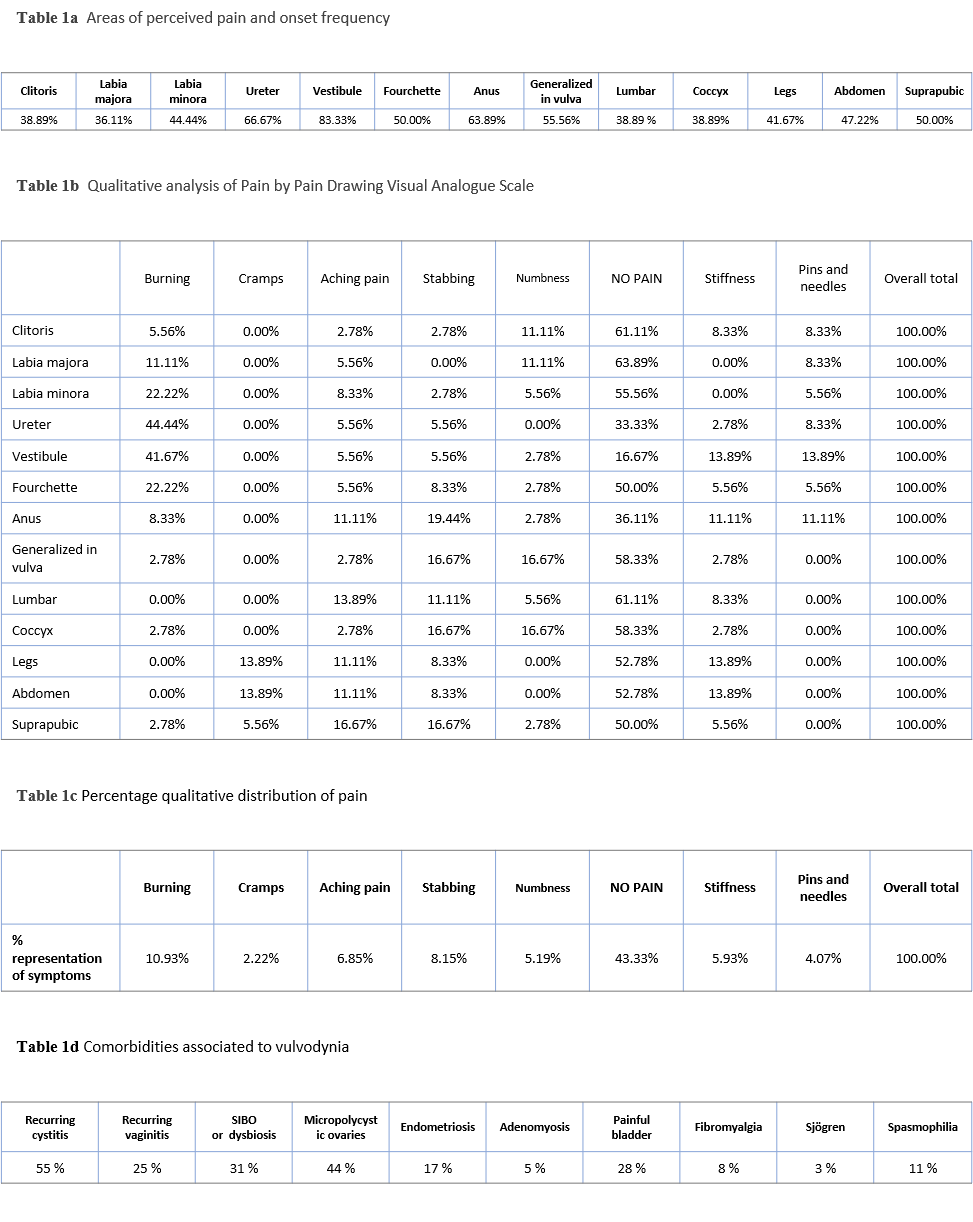
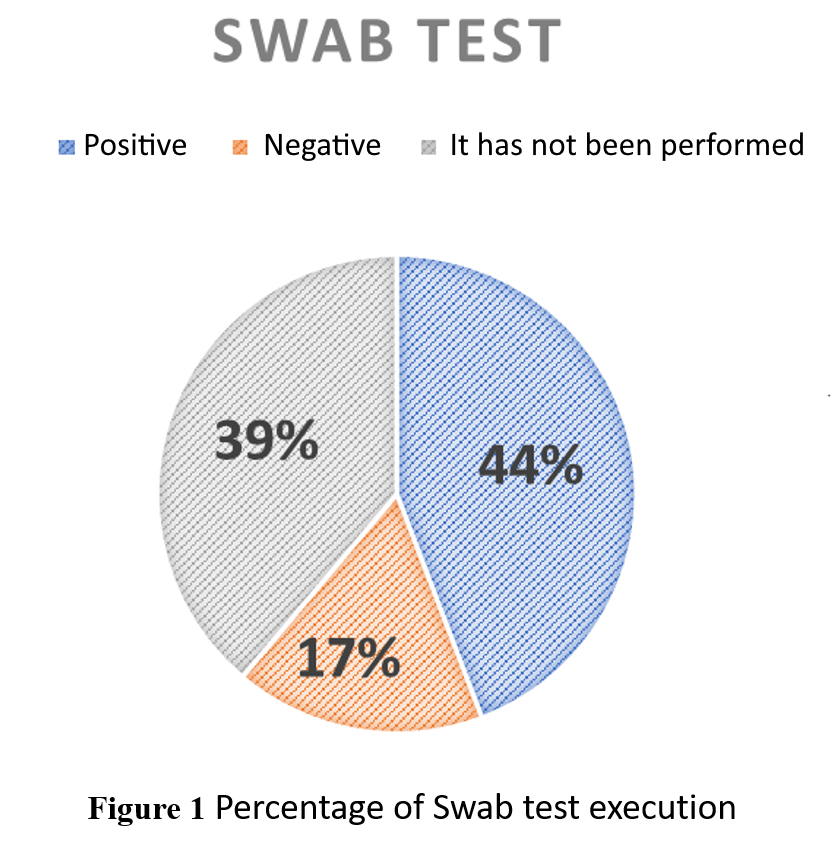
The study involved 72 women with vulvodynia presenting comorbidities, e.g. endometriosis (Table 1d). Among them, 19% had provoked vulvodynia, 28% had unprovoked, and 53% had mixed type. Among the participants, 61% underwent the Swab Test, a diagnostic procedure for vulvodynia, resulting in 44% positive and 17% negative outcomes (Figure 1). The body chart was valuable in visualizing pain patterns, revealing a prevalence of burning, stabbing, and dull pain rather than the commonly depicted “pins and needles” sensation (Figure 2, Table 1b and 1c). Concerning pain perception, 39% of patients reported pain in the lumbar region (Table 1a), but only 4.2% mentioned pre-existing low back pain before vulvodynia onset. The NPRS score indicated a significant intensity of pain experienced by the participants (M t0 = 8.667, SD t0 = 1.163).
Discussion and Conclusion
The study found a high percentage of non-execution of the SWAB test, possibly due to confusion regarding different execution methods reported in the literature or doubts about its relevance in confirming vulvodynia. [3] The qualitative presentation of pain differs from the common descriptions. Identifying the pain quality helps understand its type (nociceptive, neuropathic, nociplastic), so physical therapists should be aware that distinct pain types require tailored multimodal and patient-centered treatments. The experience of referred pain in distant areas and the occurrence of comorbidity suggests potential sensitization (Figure 2 and Table 1d). [ 4 ] In conclusion, this study underscores the importance of a comprehensive assessment of vulvodynia, considering both quantitative and qualitative aspects of pain, to enhance diagnosis and management strategies for affected women.
REFERENCES
- Chalmers KJ, Catley MJ, Evans SF, Moseley GL. Clinical assessment of the impact of pelvic pain on women. Pain. 2017;158(3):498-504. doi:10.1097/J.PAIN.0000000000000789
- Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet Gynecol. 2016;127(4):745-751. doi:10.1097/AOG.0000000000001359
- Vieira-Baptista P, Lima-Silva J, Beires J, Donders G. Women without vulvodynia can have a positive ‘Q-tip test’: a cross sectional study. Journal of Psychosomatic Obstetrics & Gynecology. 2017 Oct 2;38(4):256-9
- Torres-Cueco R, Nohales-Alfonso F. Vulvodynia—It Is Time to Accept a New Understanding from a Neurobiological Perspective. Int J Environ Res Public Health. 2021;18(12). doi:10.3390/IJERPH18126639