La scala di Berg è uno strumento adeguato alla misurazione dell’equilibrio nelle persone con sclerosi multipla e avanzata disabilità nel cammino: evidenze dall’analisi di Rasch
The Berg Balance Scale is a proper tool to measure balance in persons with Multiple Sclerosis and an advanced walking disability: evidence from Rasch analysis
Introduction
Persons with Multiple Sclerosis (PwMS) are at high risk of falling, and falls are proven to be consistently associated with balance impairment.
The Berg Balance Scale (BBS) is one of the most widely used tools to assess balance in PwMS, also within RCTs. Reliability and validity of the BBS in PwMS were evaluated through the Classical Theory Test (concurrent validity with Dynamic Gait Index (r=0.780) and the Timed-Up-and-Go test (r=0.620). It discriminated with a low sensitivity between fallers and non-fallers. Inter-rater and intra-rater reliability were excellent (ICC=0.960).
Unfortunately, these traditional psychometric procedures cannot assess some crucial requirements underlying the use of rating scales such as the BBS. Indeed, Rasch analysis has emerged as a powerful tool to evaluate the measurement quality of a scale.
Hence, this study aims to evaluate the BBS measurement properties in a multicenter sample of PwMS through Rasch analysis.
Methods
Data were collected retrospectively within the outpatient Neuro-rehabilitation services of three Italian centers for 814 PwMS, adhering to these inclusion criteria: clinically or laboratory-definite multiples sclerosis; ability to stand independently for more than 3 seconds. For each participant, we collected the BBS, the Expanded Disability Status Scale (EDSS), the Activity-specific Balance Confidence (ABC) scale, and the number of falls (previous two months).
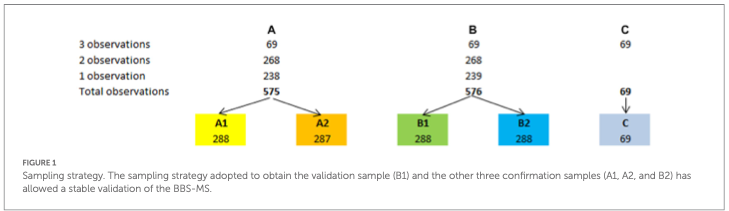
Using the Confirmatory Factor Analysis and Mokken Analysis, a preliminary unidimensional analysis of the BBS total sample (1220 observations) was performed. The sample was splitted into one validating (B1) and three confirmatory subsamples (Figure 1). Following the Rasch analysis performed on B1, item estimates were exported from B1 and anchored to the other subsamples.
Then, we studied the convergent and discriminant validity of the scale (BBS-MS) with the three external indicators.
Results
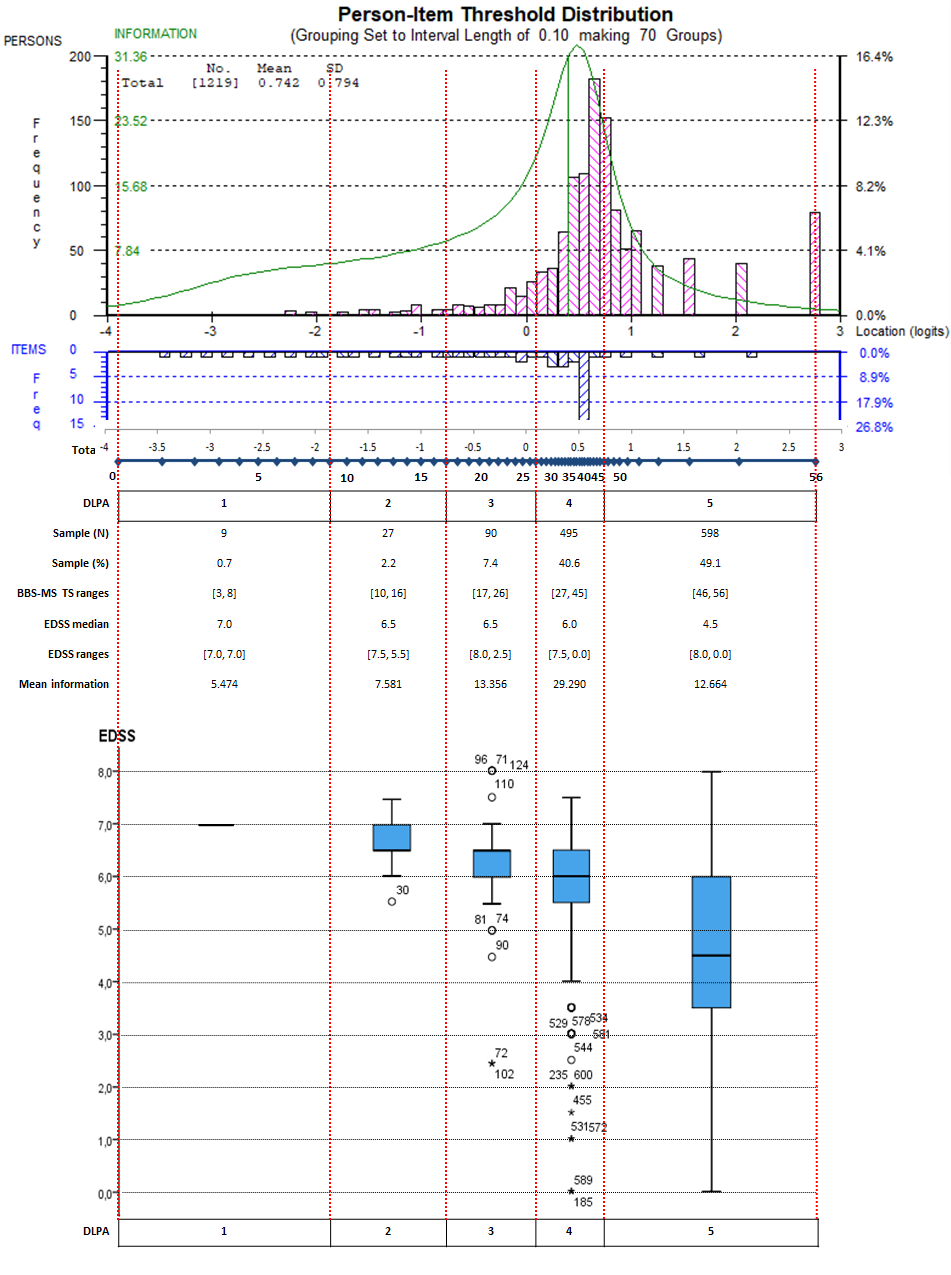
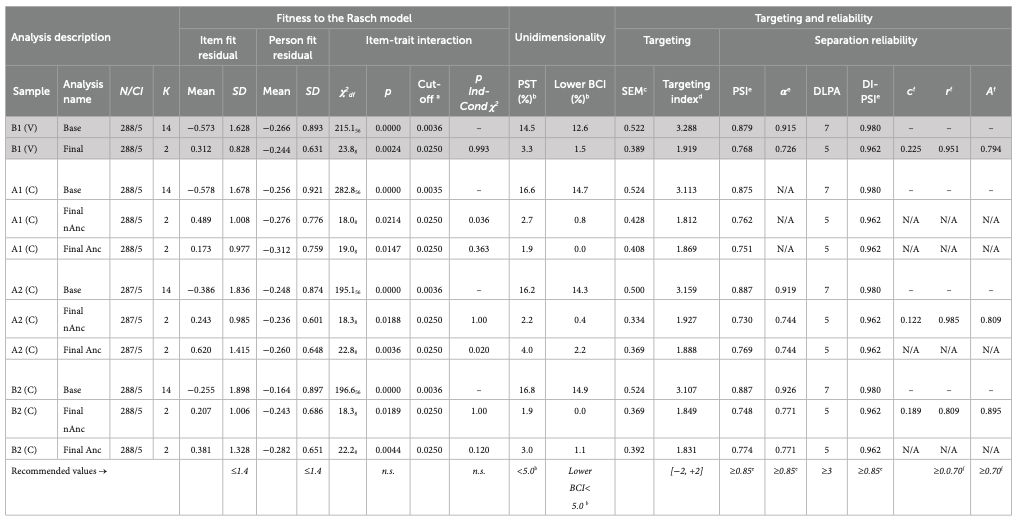
CFA and MA showed sufficient preliminary unidimensionality. The Rasch analysis on B1 failed monotonicity, local independence, and unidimensionality, and did not fit the Rasch model. After grouping locally dependent items, the BBS-MS fitted the model (χ2df=23.88; p=.003) and satisfied all requirements for adequate internal construct validity (ICV) (Table 1). However, it was mistargeted to the sample (targeting index=1.922), with a distribution-independent Person Separation Index equal to 0.962, sufficient for individual measurements (Figure 2). The B1 final solution was replicated on A1, A2, and B2 subsamples, and the B1 item estimates were anchored to the confirmatory subsamples, satisfying the fit to the model (χ2=[19.0, 22.8], p-value=[.015, .004]) and all ICV requirements (Table 2).
BBS-MS directly correlated with the ABC scale (rho=.523) and inversely with EDSS (rho=-.573). It significantly differed across groups based on the EDSS, the ABC scale, and the number of falls.
Discussion and Conclusion
To our knowledge, this is the first study reporting on the Rasch analysis of the BBS for PwMS. It supports the ICV, reliability, and targeting of the BBS-MS as a measurement tool in an Italian multicentre sample of PwMS. Using one validation and three confirmation subsamples, we demonstrated the BBS-MS fitting to the Rasch model and the satisfaction of all requirements for adequate ICV.
On the other hand, the scale was slightly mistargeted to our convenience sample as its items were, on average, less difficult than the mean ability of the sample, uncovering significant targeting issues for a precise balance measurement in still ambulatory PwMS.
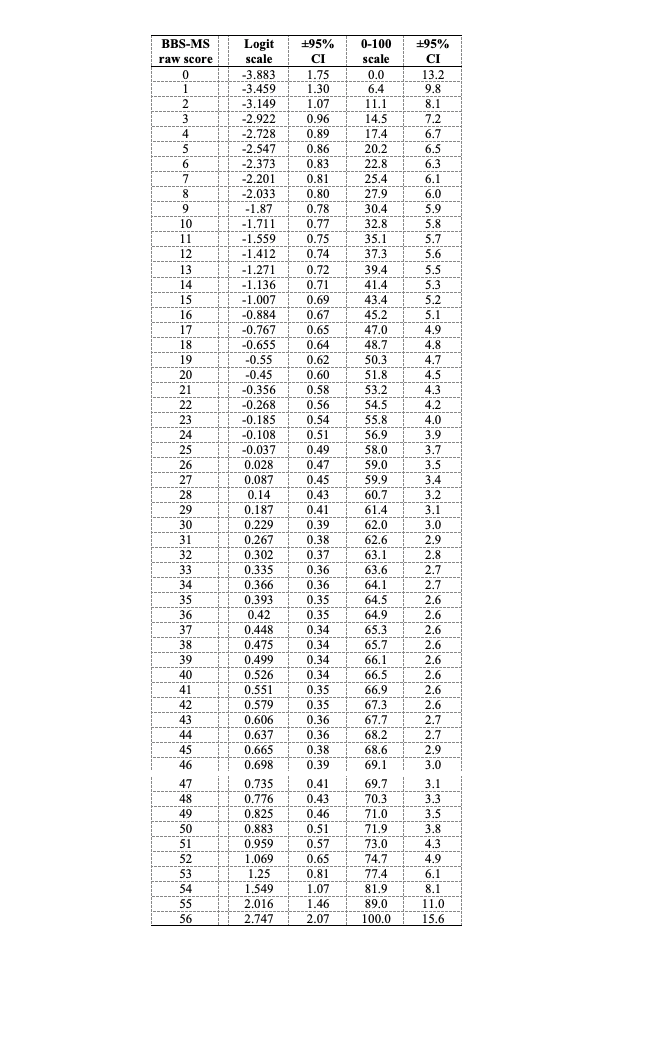
Indeed, our study suggested that the BBS-MS may be a precise and responsive measurement scale to assess balance in RCTs targeted to more disabled PwMS with an advanced walking disability. Thanks to this validation, we provided interval-level measures of balance ability, allowing parametric statistics to be used.
REFERENCES
- Nilsagard, C. Lundholm, E. Denison, and L.G. Gunnarsson, Predicting accidental falls in people with multiple sclerosis — a longitudinal study. Clin Rehabil 23 (2009) 259-69
- V. Jacobs, and S.L. Kasser, Balance impairment in people with multiple sclerosis: preliminary evidence for the Balance Evaluation Systems Test. Gait & posture 36 (2012) 414-8.
- Cattaneo, J. Jonsdottir, and S. Repetti, Reliability of four scales on balance disorders in persons with multiple sclerosis. Disability and rehabilitation 29 (2007) 1920-5.
- Hobart J, Cano S. Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods. Health Technol Assess 13 (2009) (12): iii, ix-x, 1-177.
- Tennant, and P.G. Conaghan, The Rasch measurement model in rheumatology: what is it and why use it? When should it be applied, and what should one look for in a Rasch paper? Arthritis Rheum 57 (2007) 1358-62.