Mobility Scale for Acute Patients: validità e affidabilità della scala in lingua italiana
Mobility Scale for Acute Patients: validity and reliability of the Italian scale
Introduction
Many well-known functional scales include items of mobility and have been validated for assessing functional status in the rehabilitation setting but propose measures of complex items, that would be expected months after an acute event. The Mobility Scale for Acute Stroke Patients (MSAS) by Simondson et al. (1996) was developed to respond to the need for a scale that addresses the specific needs of neurological patients in the acute setting. Although the MSAS was developed to specifically discriminate between the lower levels of mobility in acute stroke patients in the first two weeks post-onset, we thought it could also be a valid tool to be used for the assessment of patients in the early sub-acute phase of stroke. The present study aims to develop and validate a version of the MSAS in Italian.
Methods
The English version of the MSAS was translated into Italian according to international guidelines. Later were tested the internal consistency, concurrent validity, reliability, and responsiveness properties of the scale. The recruited patients were divided into two groups. For the scute (AC) group we recruited patients admitted for rehabilitation within 14 days of the stroke onset, while for the sub-acute (SA) group, we recruited patients admitted for rehabilitation between 15 and 90 days after the stroke. Each patient was tested twice after 24 hours by the same physical therapist to evaluate the test-retest reliability. To assess inter-rater reliability, two blinded physical therapists independently evaluated the same person. To investigate the responsiveness the MSAS was administered at the time of admission and two (acute) and seven (sub-acute) weeks later, at the discharge, to a sub-group of 44 patients.
Results
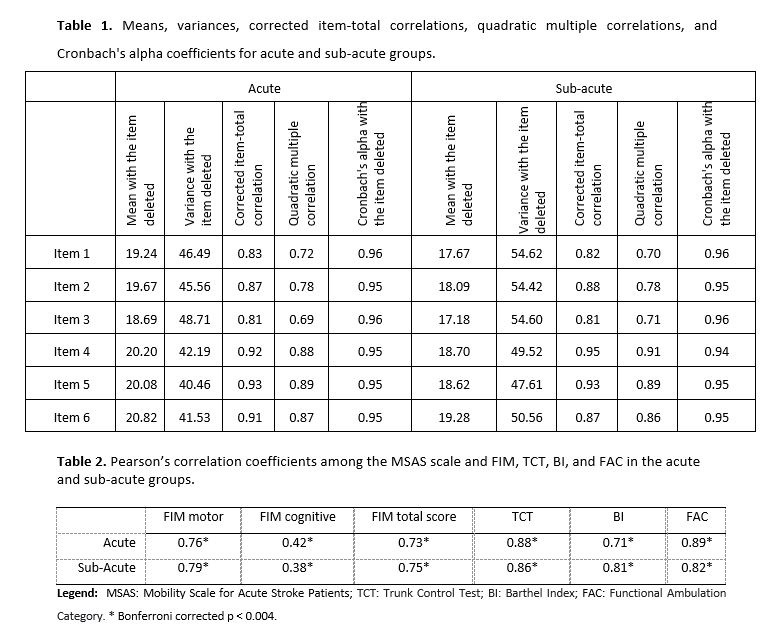
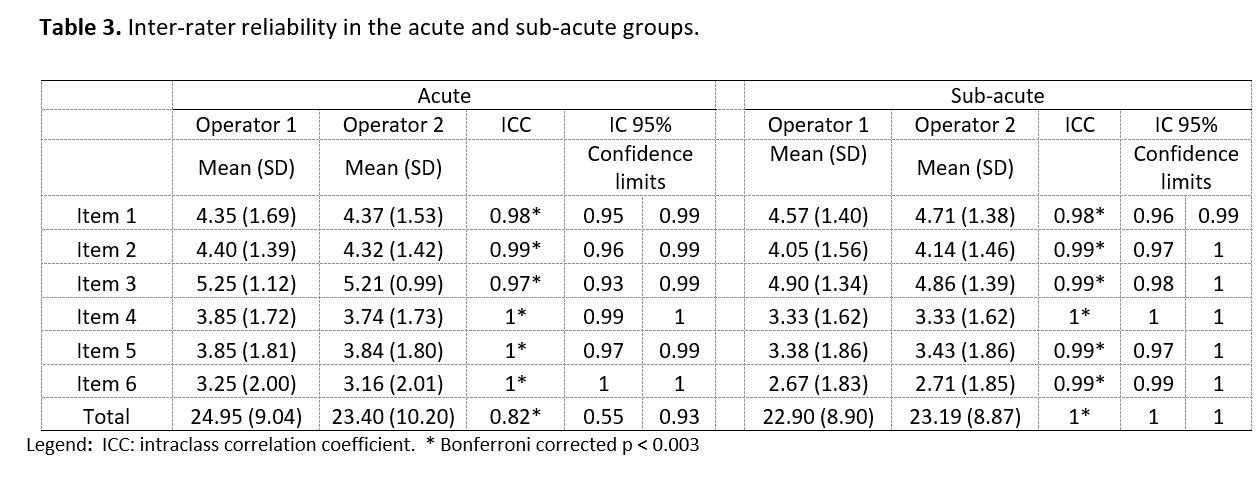
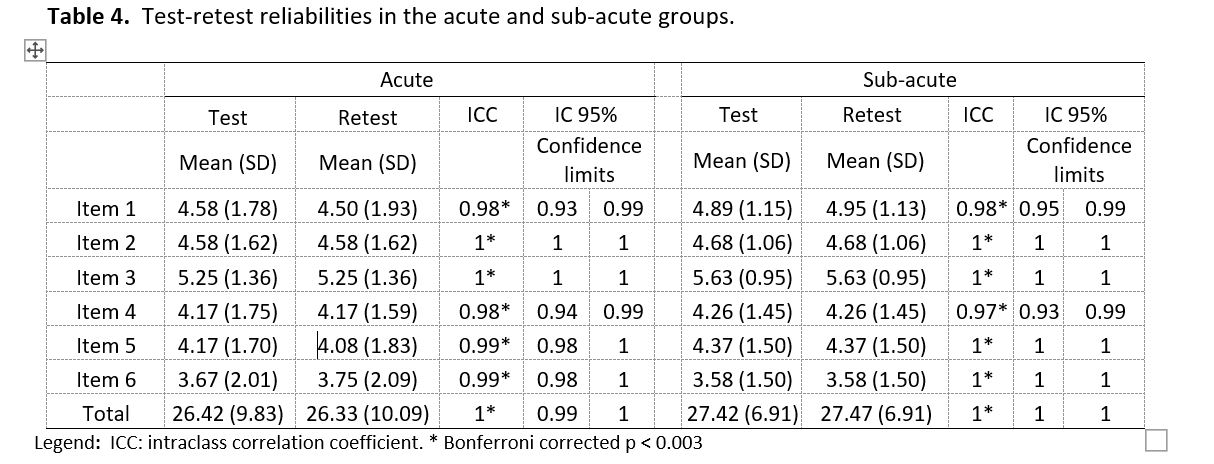
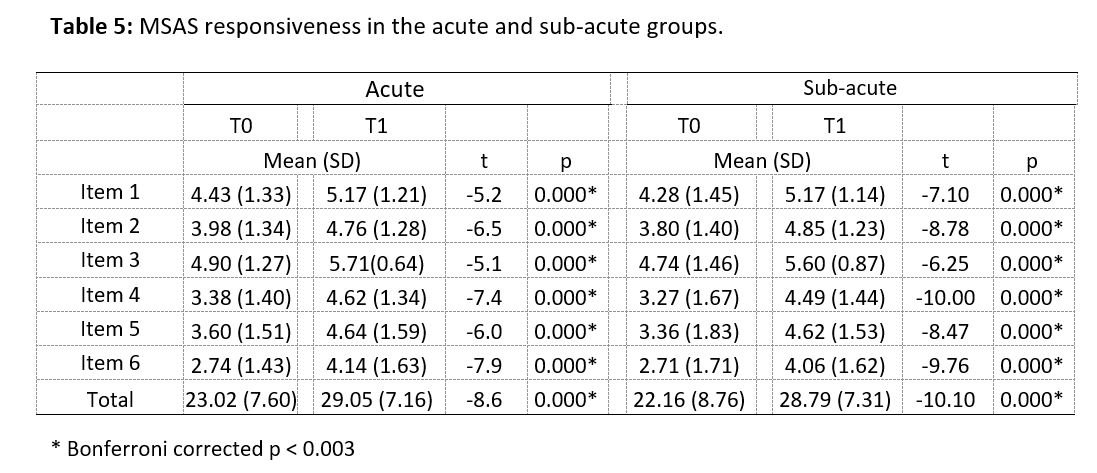
Internal consistency results showed statistically significant data for both groups. Cronbach’s alpha for individuals in AC and SA phases showed values equal to 0.96, and the alpha deleted analysis (Table 1) demonstrates that all the items on the scale have reason to exist. Concurrent validity showed statistically significant data for both populations. Indeed, we obtained statistically significant data for all scales (Table 2). The Italian version of the MSAS showed significant and high intra-rater reliabilities (all ICCs ≥ 0.75) for both the AC and SA sub-groups (Table 3). The MSAS also showed excellent test-retest reliabilities (all ICCs ≥ 0.90) for the AC and SA sub-groups (Table 4). The reactivity of the scale, evaluated through the Student’s ts for paired samples on the sub-sample of 42 individuals, showed statistically significant improvements over time for all items and the total scale (Table 5).
Discussion and Conclusion
The results show that the scale is stable and reliable both in the evaluation after 24 hours and in the evaluation between different operators. A high internal consistency and a strong correlation between the scales used as Gold Standard and the MSAS were found for both acute and sub-acute samples. The scale has also proved to be able to evaluate the improvement obtained by patients following the rehabilitation treatments carried out.
REFERENCES
- Simondson J, Goldie P, Brock K, Nosworthy J. The Mobility Scale for Acute Stroke Patients: intra-rater and interrater reliability. Clin Rehabil 1996; 10: 295–300. F
- Simondson JA, Goldie P, Greenwood KM. The Mobility Scale for Acute Stroke Patients: concurrent validity. Rehabil. 2003 Aug;17(5):558-64. doi: 10.1191/0269215503cr650oa. PMID: 12952164.
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, et al. (2005) Principles of good practice for the translation and cultural adaptation process for patient-reported outcome (PRO) measures: report of the ISPOR task forces for translation and cultural Value Health 8: 94-104.