Cammino e fatica nelle Persone con Sclerosi Multipla: Strategie compensatorie per regolare la clearance nella fase di metà volo. Uno studio qualitativo.
Walking and fatigue in People with Multiple Sclerosis: Gait compensatory strategies to control clearance during the mid-swing phase. A qualitative study.
Introduction
People with Multiple Sclerosis (PwMS) commonly experience falls or near falls, of which one-third seem to be associated with fatigue or tripping. Lately, different studies have inquired about changes in gait parameters related to fatigue, but none have depicted the clinical compensations in the swinging limb that PwMS implement when they get fatigued, to reduce the risk of tripping. The present study tries to describe the strategies that PwMS carry out to control the clearance of the swinging limb when they get fatigued.
Methods
Thirty-two PwMS (EDSS 3.0±1.5) and 8 healthy subjects (HS) were recruited. Kinematic data were collected using a SMART-D motion capture system (BTS, Milano, Italy) with LAMB protocol. Subjects were asked to walk continuously at a steady cadence (spontaneous + 15%) suggested by a metronome. Every minute physical exertion was recorded on the Borg scale (RPE); the test ended as the subject reached a score of 17 (very hard).
We estimated the trend over time for clearance, foot drop, and lower limb length (LL), calculated as the distance between the ipsilateral anterior superior iliac spine and lateral malleolus. For each variable, we derived the slope trends and considered the slope coefficient (k) to describe our findings.
Finite mixture models were used to provide a cluster analysis: a) Univariate model of k clearance; b) Multivariate model of k-LL and k-footdrop, considering the subjects with a negative clearance according to the previous univariate analysis.
Results
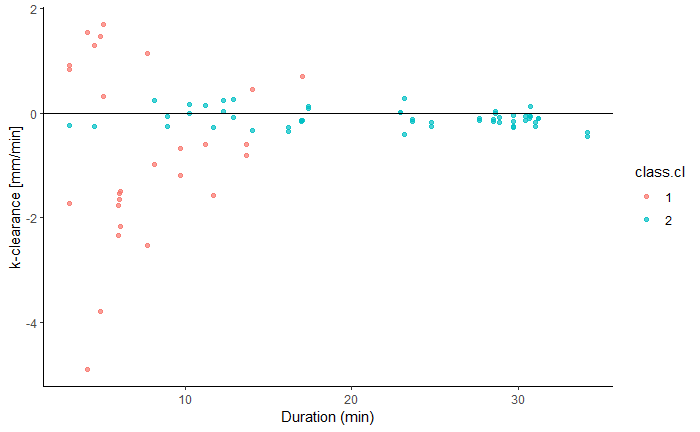
PwMS walked less time (13.9±10.22 vs 30.0±1 min) HS reaching an RPE of 17, while HS walked 30 minutes reaching an RPE≤11. The cluster analysis of the k clearance showed 2 different patterns (Figure 1): 1a) showing a minimal clearance variability -0.11(0.03)mm/min (light-blue dots); 1b) a higher clearance variability -0.62(1.1)mm/min (red dots).
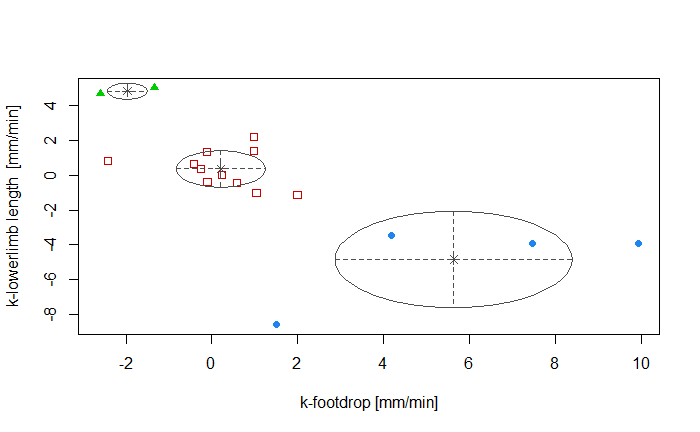
The multivariate model (Figure 2), considering subjects in 1b) and with a negative k-clearance, showed 3 different patterns related to k-LL and k-footdrop: the first group (green triangles) had an increased LL over time (k-LL=4.8(0.5)mm/min) and a reduction in the foot drop (k-footdrop=-2.0 (0.5)mm/min). The second group (red squares) showed a minimal variation in both parameters (k-footdrop=0.2(1.0)mm/min, k-LL = 0.3(1.0)mm/min). The third group (blue dots) had an increased k-footdrop (5.6(2.8)mm/min) associated with a reduction in the LL (k-LL=-4.8 (2.8)mm/min).
Discussion and Conclusion
The present findings seem to have the potential to better guide gait rehabilitation. In subjects with a stable clearance, the fatiguability seems associated more to deconditioning and general stability. For subjects who increase clearance (over-compensating), the treatment could be aimed toward more energy-conservative strategies. While, for subjects more at risk of tripping we found three different patterns: a group had a progressive deficit in ankle dorsiflexion partially compensated by a shortening of the limb in flight; another group had a slight change in both; finally, a third group had a deficit related to limb length in flight partially compensated by an increase in ankle dorsiflexion. Thus, rehabilitation intervention could be directed to proximal or, distal muscle function or both, and ankle-orthosis prescription could be suggested to subjects with a real need. Other factors (eg. trunk, pelvis) should be explored in future studies.
REFERENCES
Comber L, Galvin R, Coote S. Gait deficits in people with multiple sclerosis: A systematic review and meta-analysis. Gait Posture. 2017 Jan;51:25-35. doi: 10.1016/j.gaitpost.2016.09.026. Epub 2016 Sep 26. PMID: 27693958.
Broscheid KC, Behrens M, Bilgin-Egner P, Peters A, Dettmers C, Jöbges M, Schega L. Instrumented Assessment of Motor Performance Fatigability During the 6-Min Walk Test in Mildly Affected People With Multiple Sclerosis. Front Neurol. 2022 May 9;13:802516. doi: 10.3389/fneur.2022.802516. PMID: 35614920; PMCID: PMC9125148.
Fritz NE, Eloyan A, Baynes M, Newsome SD, Calabresi PA, Zackowski KM. Distinguishing among multiple sclerosis fallers, near-fallers and non-fallers. Mult Scler Relat Disord. 2018 Jan;19:99-104. doi: 10.1016/j.msard.2017.11.019. Epub 2017 Nov 22. PMID: 29182996; PMCID: PMC5803437.