Ci sono differenze di sesso e genere negli interventi valutati dagli studi randomizzati controllati sulla lombalgia? Uno studio di meta-ricerca
Are there sex and gender differences in low back pain interventions of randomized controlled trials? A meta-research study
Introduction
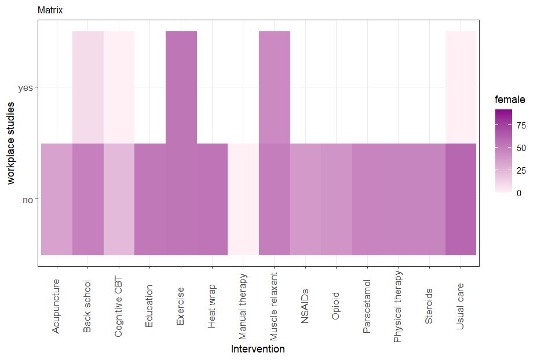
Low back pain (LBP) is the leading cause of Years Lived with Disability worldwide. The global prevalence of LBP is higher among females compared with males across all age groups (1). To improve LBP management, various rehabilitation interventions recommended by high quality clinical practice guidelines are effective (2). However, treatment effects can be different in male and female. This can also depend on the recruitments of participants in the randomized controlled trials (RCTs). Thus, we investigated the prevalence of different sex and gender participants in LBP trials to improve knowledge in sex and gender differences, enhancing tailored healthcare and external validity of randomized controlled trials.
Methods
Results
Discussion and Conclusion
REFERENCES
1. Collaborators GBDLBP. Global, regional, and national burden of low back pain, 1990-2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(6):e316-e29.
2. Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, van Tulder M, Koes BW. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J. 2018 Nov;27(11):2791-2803.
3. Gianola S, Bargeri S, Del Castillo G, Corbetta D, Turolla A, Andreano A, et al. Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Br J Sports Med. 2022;56(1):41-50.