Il rapporto armonico è l’indice di cammino derivato dall’accelerazione del tronco più reattivo alla riabilitazione nelle persone con malattia di Parkinson in stadi moderati della malattia.
Harmonic ratio is the most responsive trunk-acceleration derived gait index to rehabilitation in people with Parkinson’s disease at moderate disease stages.
Introduction
Harmonic ratios (HRs), recurrence quantification analysis in the antero-posterior direction (RQAdetAP), and stride length coefficient of variation (CV) have recently been shown to characterize gait abnormalities and fall risk in people with Parkinson’s disease (pwPD) at moderate disease stages. This study aimed to i) assess the internal and external responsiveness to rehabilitation of HR, RQAdetAP, and CV, ii) identify the baseline predictors of normalization of the gait stability indexes, and iii) investigate the correlations between the gait indexes modifications (∆) and clinical and kinematic ∆s in pwPD at Hoehn and Yahr disease staging classification 3.
Methods
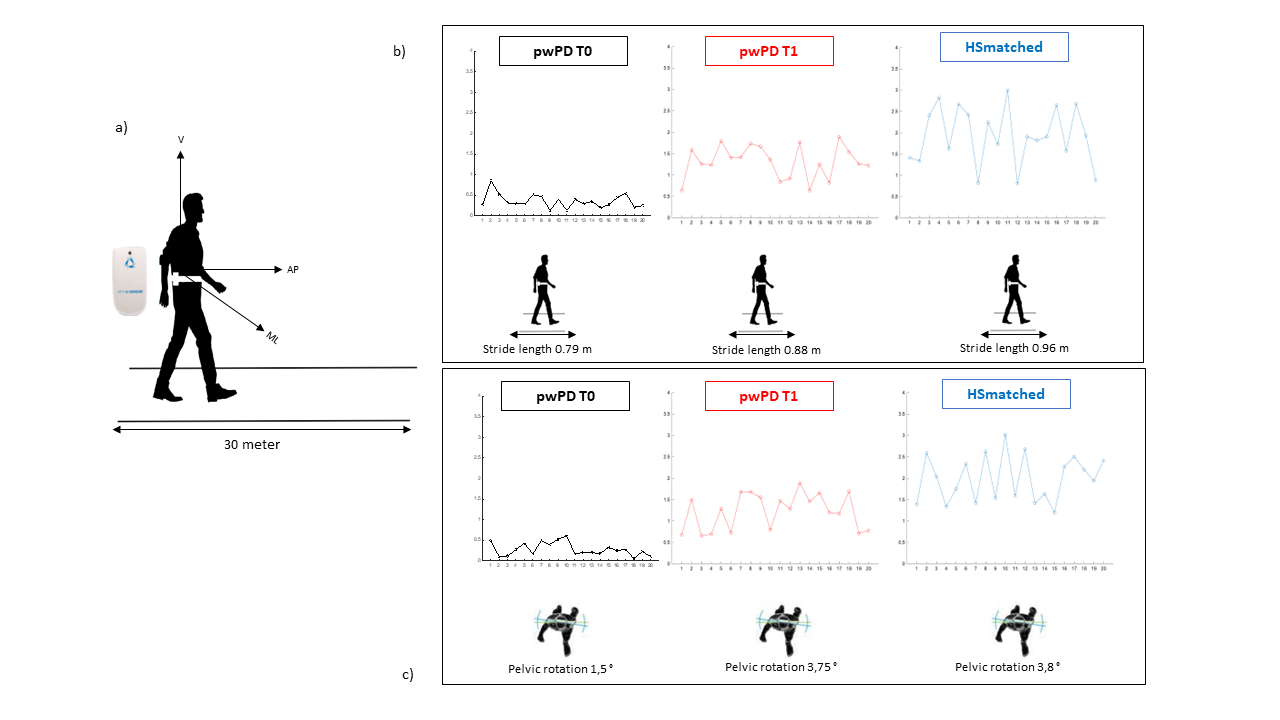
The trunk acceleration patterns of 21 pwPD and 21 age- and speed-matched healthy subjects (HS) were acquired during gait using an inertial measurement unit at baseline (T0). pwPD were also assessed after a 4-week rehabilitation period (T1). Each participant’s HR in the antero-posterior (HRAP), medio-lateral (HRML), and vertical directions, RQAdetAP, CV, spatio-temporal, and kinematic variables were calculated. Unpaired t-test or Mann-Whitney test and Cohen’s d were used to identify significant differences between pwPD and HS at T0 and normalization at T1. Multiple linear regression analysis was performed to identify the predictors of improvement. Partial correlation analysis adjusting for Δgait speed was performed between the Δs. Area under the ROC curves (AUCs) and minimally clinically important differences (MCID) were calculated to assess external responsiveness.
Results
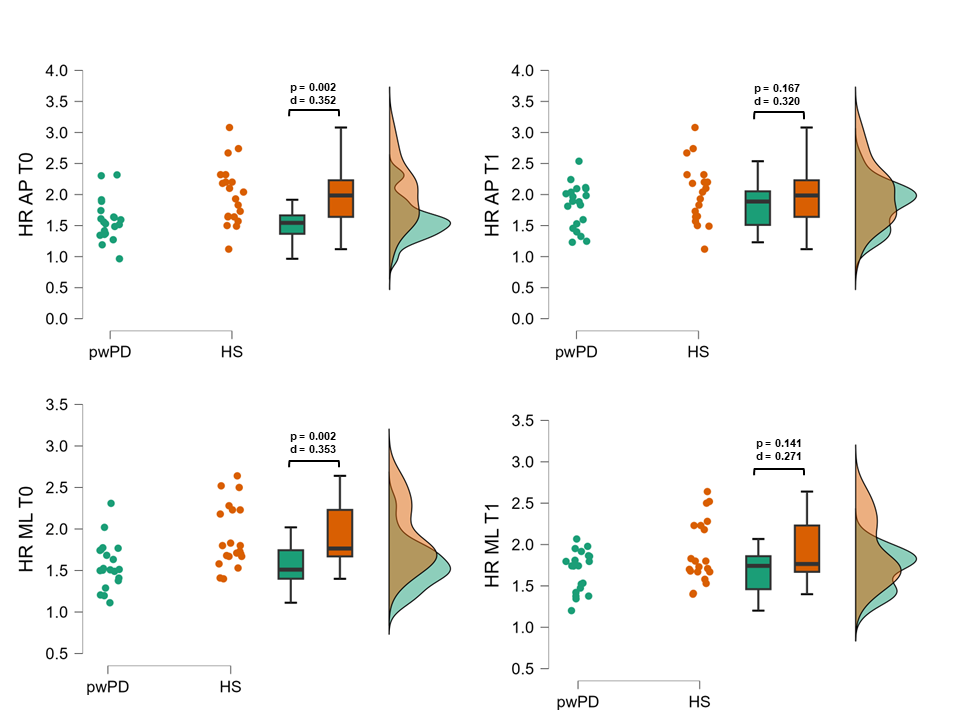
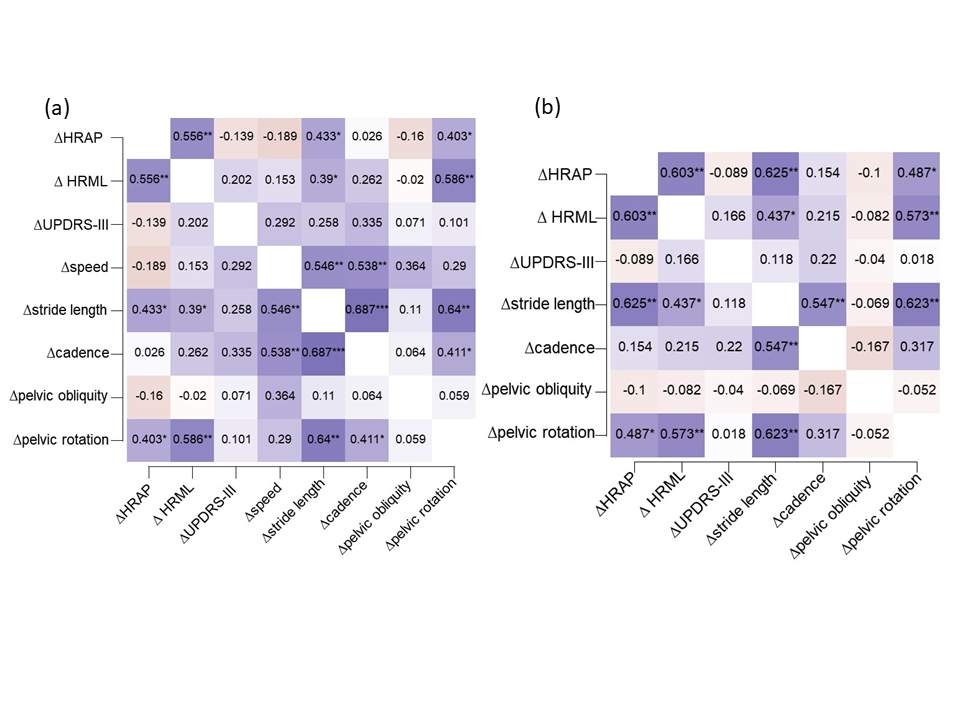
After rehabilitation, pwPD improved in HRAP, HRML, gait speed, stride length, cadence, pelvic obliquity, pelvic rotation, and UPDRS-III, with medium-to-large effect sizes (0.52 > d < 0.82). At T1, HRAP, HRML, stride length, and pelvic rotation were no longer different from HS, suggesting a normalization of these parameters (Fig. 1). Lower HRs and higher pelvic rotation values at baseline predicted ∆HRs. ΔHRAP correlated with ΔHRML, Δstride length and Δpelvic rotation, regardless of Δgait speed (Fig. 2). ΔHRAP ≥ 21.47 %, Δstride length ≥ 10.09 %, and Δpelvic rotation ≥ 8.59 %, respectively, were required to normalize HRAP with 95 %, 88 %, 74 %, and 81 % probability. ΔHRML ≥ 36.94 %, Δstride length ≥ 22.67 %, and Δpelvic rotation ≥ 37.67 %, were required to normalize HRML with 92 %, 71 %, 73 %, and 90 % probability. RQAdetAP and step length CV were not responsive to rehabilitation.
Discussion and Conclusion
HRAP and HRML improved to normative values after rehabilitation and showed high internal and external responsiveness. When using inertial measurement units, HRAP and HRML can be considered as responsive outcome measures for assessing the effectiveness of rehabilitation on trunk smoothness during walking in pwPD at moderate disease stages. Subjects with reduced trunk mobility at baseline were more likely to improve their HRs and focusing on exercise programs on pelvic rotation and stride length (Fig. 3) could optimize the rehabilitative planning in order to tailor gait interventions in pwPD at moderate disease stages.
REFERENCES
Castiglia, Stefano Filippo et al. “Ability of a Set of Trunk Inertial Indexes of Gait to Identify Gait Instability and Recurrent Fallers in Parkinson’s Disease.” Sensors (Basel, Switzerland) vol. 21,10 3449. 15 May. 2021, doi:10.3390/s21103449
Trabassi, Dante et al. “Machine Learning Approach to Support the Detection of Parkinson’s Disease in IMU-Based Gait Analysis.” Sensors (Basel, Switzerland) vol. 22,10 3700. 12 May. 2022, doi:10.3390/s22103700
Serrao, Mariano et al. “Prediction of Responsiveness of Gait Variables to Rehabilitation Training in Parkinson’s Disease.” Frontiers in neurology vol. 10 826. 2 Aug. 2019, doi:10.3389/fneur.2019.00826
Hubble, Ryan P et al. “Trunk Exercises Improve Gait Symmetry in Parkinson Disease: A Blind Phase II Randomized Controlled Trial.” American journal of physical medicine & rehabilitation vol. 97,3 (2018): 151-159. doi:10.1097/PHM.0000000000000858