Fisioterapia in paziente con mielopatia cervicale dopo microdiscectomia cervicale, Gait Analisys e stabilometria: un caso clinico
Physical Therapy in patient with cervical mielopathy following cervical microdiscectomy, gait analysis and stabilometry results: a case report
Introduction
Degenerative cervical myelopathy (DCM) is a progressive, degenerative condition, which is a consequence of degeneration and structural changes of the intervertebral disks that may lead to structural and vascular changes to the spinal cord.1 Symptoms may present as hyperreflexia, clumsiness in gait,neck stiffness, shoulder pain, paresthesias, or radiculopathic signs.1 Surgical intervention is recommended for patients with moderate and severe DCM.2 There are no rigorous studies evaluating if physiotherapy causes benefit or harm after surgical decompression in patients with DCM.3
With this case report we describe the results obtained in a patient with DCM after surgical decompression who received standard physiotherapy for trunk control according to the Bobath concept, global muscle strengthening especially in the lower limbs and balance training and gait training associated to Virtual Reality.
Methods
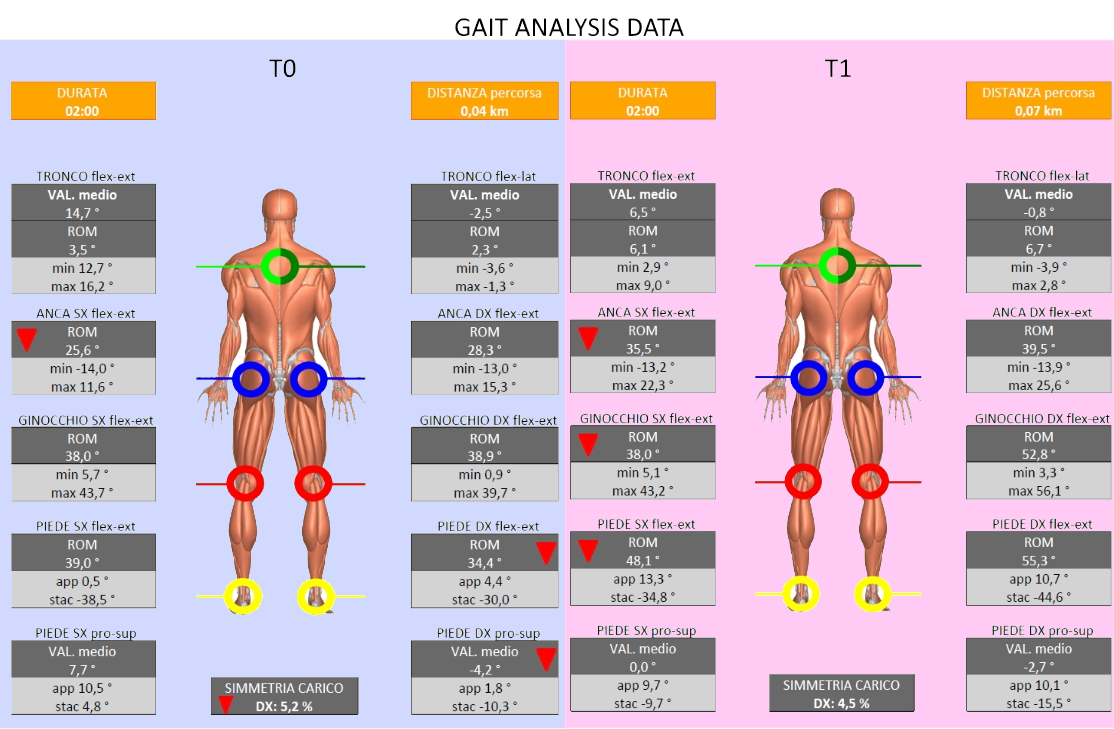
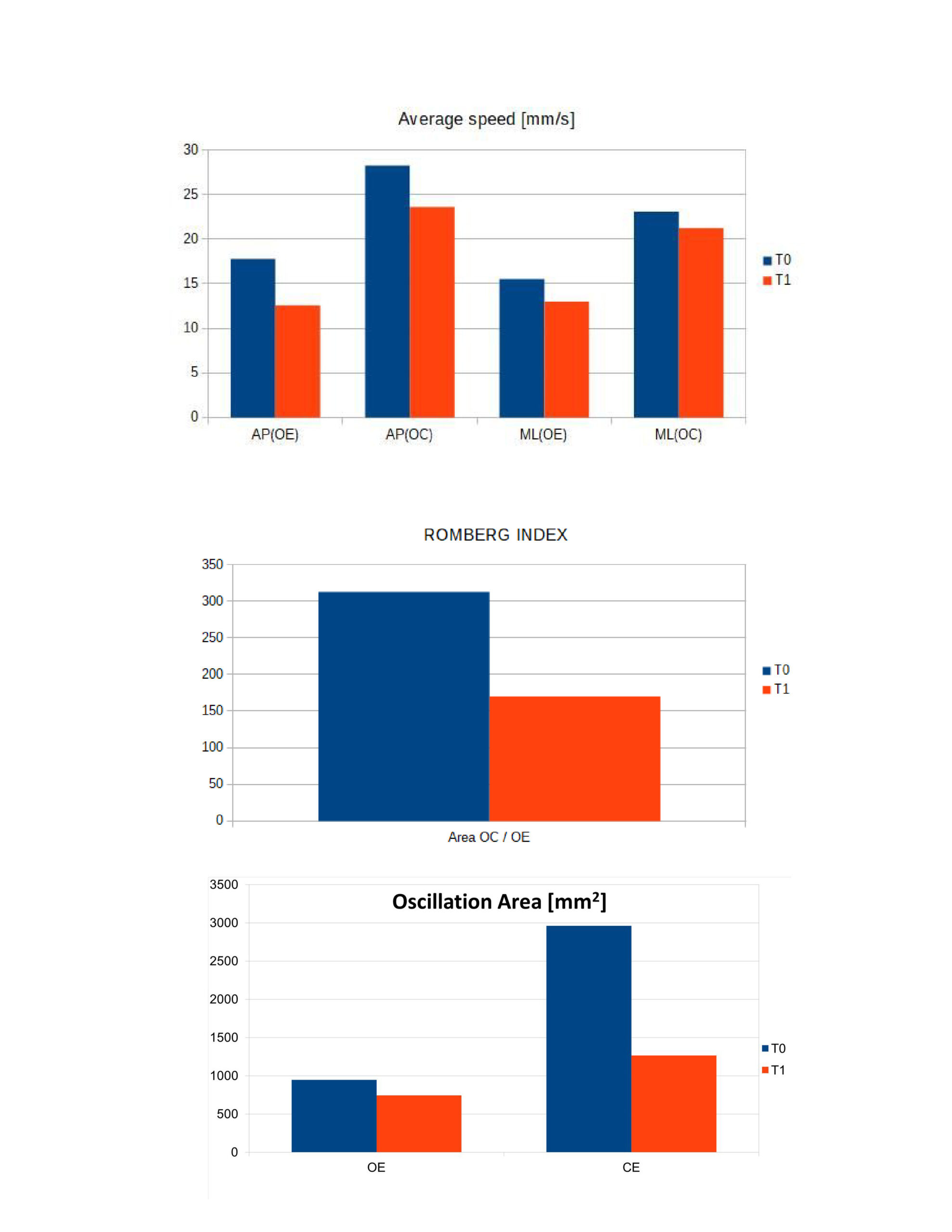
A 68 year old man, with severe DCM, MJOA 12 (modified Japanese Orthopaedic Association scale), arrived after surgical intervention. At T0 the patients had a slight left hemiparesis, Mingazzini positive for LL levelling, F4 proximal sthenic deficit, reported left hand paraesthesia. He could walk with a 4-wheeled walker, had reduced LL major control on the left. The tests included: open/closed eyes balance with stabilometric platform (D-Wall, Tecnobody), the outcomes included parameters of center of pressure (COP) during quiet standing; Gait Analysis (WALKER VIEW, Tecnobody) was possible leaning on the handrail, the outcomes included velocity, stride length and joints Range of Motion. The treatment (lasted 3 months, three days a week) focused on balance training with real time biofeedback on stabilometric platform, stable and unstable surfaces; gait training through treadmill with real-time feedback.
Results
The stabilometric parameters have improved: there was reduction of the oscillation area OE 21% and 57% in OE and CE test (mm²: T0 OE 945.92 CE 2959.33 – T1 OE 742.99 CE 1263.97). Romberg index decreased (Area CE/OE T0 313, T1 170). The average speed AP decrease about 34% OE and 17% EC (mm/s T0 OE 17,78 CE 28,24 T1 OE 12,58 CE 23,60). The average speed LL decrease about 17% OE and 8% CE (mm/s T0 OE 15,55 CE 23,09 T1 OE 12,99 CE 21,24) Gait analysis shows better trunk position in the sagittal plane (flex-ext T0 14.7°, T1 6 ,5°) and less oscillation in the frontal plane (lat-flex T0 -2.5°, T1 -0.8). An increased of the 180% of the speed (km/h: T0 1.2, T1 2.2). Improved length gait of 130% for the left, 32% right (cm: T0 l 19 r 28, T1 l 44 r 37). Improvement of parameters of step (flex-ext in stance [°] T0 l 0.5 r 4.4 T1 l 13.3 r 10 ,7, flex-ex in toe off [°] T0 l -38,5 r -30,0 T1 l -34,8 r -44,6. MJOA improved from 12 to 15.
Discussion and Conclusion
Gait impairment constitutes the most prominent clinical manifestation of cervical myelopathy, and thus its amelioration may have tremendous impact on the recovery of patients’ functionality.4 Individuals with DCM shown a greater postural sway with increased muscle activation in the trunk and lower extremities during quiet standing.The treatment through a real time biofeedback stabilometric platform, and through gait training led to an improvement in the kinematic parameters of the gait and in the parameters related to the COP. All this has allowed the rehabilitation team and the patient himself to objectively verify the changes obtained throughout the training to direct the treatment towards the limits identified during the sessions and allowing the patient to establish active coping strategies. Future works may provide follow-ups to verify the maintenance of the obtained results.
REFERENCES
1. Cook, Chad E., et al. “Clinical tests for screening and diagnosis of cervical spine myelopathy: a systematic review.” Journal of manipulative and physiological therapeutics 34.8 (2011): 539-546.
2. Fehlings, Michael G., et al. “A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression.” Global spine journal 7.3_suppl (2017): 70S-83S.
3. Tetreault, Lindsay, et al. “Significant predictors of outcome following surgery for the treatment of degenerative cervical myelopathy: a systematic review of the literature.” Neurosurgery Clinics 29.1 (2018): 115-127.
4. Siasios, Ioannis D., et al. “The role of gait analysis in the evaluation of patients with cervical myelopathy: a literature review study.” World Neurosurgery 101 (2017): 275-282.