PRATICA CLINICA FISIOTERAPICA INFORMATA DALLA TERAPIA BASATA SULL’ACCETTAZIONE E L’IMPEGNO (ACT) NEL NON-SPECIFIC CHRONIC LOW BACK PAIN (NSCLBP): A CASE-REPORT
ACCEPTANCE AND COMMITMENT THERAPY (ACT) INFORMED PHYSIOTHERAPY PRACTICE IN NON-SPECIFIC CHRONIC LOW BACK PAIN (NSCLBP): A CASE-REPORT
Introduction
Non-specific chronic low back pain (NSCLBP) is a common condition and source of significant suffering, disability and healthcare costs1.
In this case-report we show the results of a combined physiotherapy treatment with the third wave generation of Cognitive Behavioural Therapy (CBT), the Acceptance and Commitment Therapy (ACT)2.
ACT has been shown to have positive effects in chronic pain3, and meta-analyses of ACT for chronic pain showed improvements in pain intensity, physical functioning, depression and anxiety, and quality of life (QoL)4.
Methods
48-year-old male industry worker with CLBP for one year.
Recently divorced, he lives with his young daughter.
His general health is fine and he enjoys cycling in the weekend.
One year ago at job during heavier work than usual, constant LBP (NRPS 5/10 at rest) spreading to the right buttock without legs’ irradiation. At MRI discal bulging from L3 to S1, without evidence of herniation.
He has continued to work (NRPS 8/10 at worst).
Aggravating factors: sitting and spine loading during lifting tasks.
Only rest reduces pain and no further neurological symptoms are present.
Psychosocial factors: worries and fear about job, guarding behaviours and notes of kinesiophobia. His sleep is disrupted because of pain.
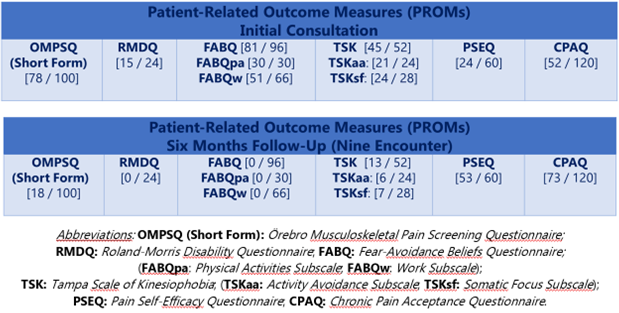
PROMs (t0 – 6/12 follow-up): OMPSQ, RMDQ, FABQ, TSK, PSEQ and CPAQ as shown in the tables: [ A1 ]
Main request: “to get strategies to manage pain and to re-establish work capacity”.
Results
The diagnostic triage5 excluded red flags for serious pathologies6 and absence of neural findings tips for diagnosis of NSCLBP.
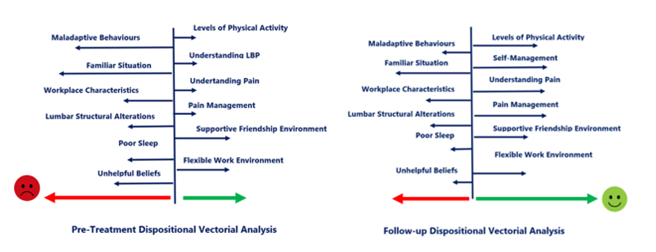
Under a dispositional framework7,8 the clinical picture -persistent stage, pain features related to mechanical behaviour with nociceptive contribution9, psychosocial aspects of fear-avoidance behaviour10 about work capacity, kinesiophobia and low self-efficacy- can be depicted in a graph with arrows showing the dispositions that tend towards manifestation and maintaining of the condition or that are preventive under a causal lens[ A2 ]
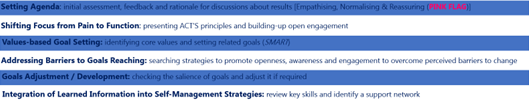
The vectorial model shows treatment goals at a glance11; it lasted 6 months, in 9 sessions, with main goals:
# make sense of pain and disability12
# expose gradually to provocative movements13
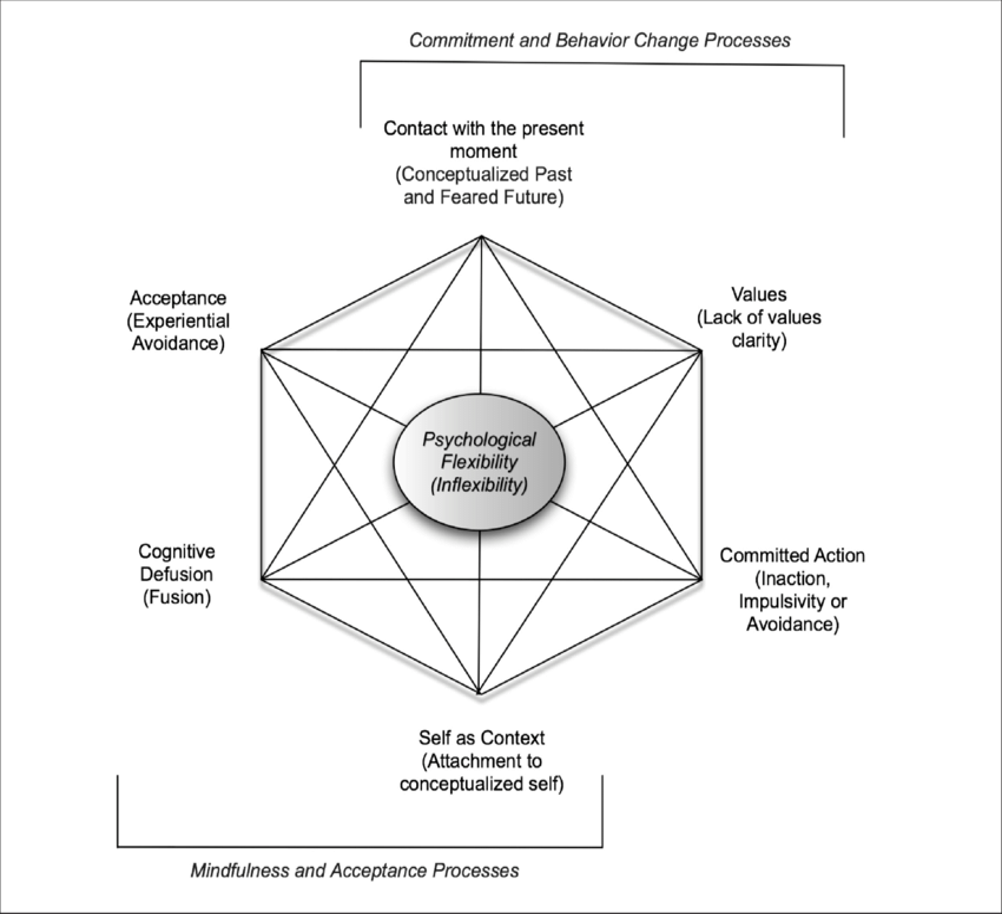
# set therapeutic path in a narrative way14 through principles of ACT, to restore patient’s autonomy and foster self-management strategies[A3,4]
Discussion and Conclusion
After different and failed rehabilitation attempts, in our episode of care it has been possible to exclude serious pathologies – and through a causal dispositionalist framework that sets apart a person-centred approach – he has been able to recover his functional levels and implement a self-management15,16 program that consent him to cope successfully with his complaint, under a shared clinical decision-making and personal empowerment lens. Further, be acquainted in ACT’s core principles, directly reduces avoidance and promotes openness, bringing the possibility to build present-focused awareness, and coordinate greater engagement in goal-oriented and values-based activities.
REFERENCES
- Murray CJL. Lancet 2012.
- Hayes SC. Behavior therapy 2004.
- Hann KEJ, McCracken LM. J Context Behav Sci 2014.
- Veehof MM. Pain 2011.
- Bardin LD. Med J Aust 2017..
- Finucane LM. J Orthop Sports Phys Ther 2020.
- Anjum RL, Copeland S, Rocca E. Rethinking causality, complexity and evidence for the unique patient: A CauseHealth resource for healthcare professionals and the clinical encounter. Springer 2020.
- Smart KM. Clin J Pain 2011.
- Vlaeyen JWS. Pain 2016.
- Lin I. Br J Sports Med 2020.
- Low M. J Eval Clin Pract 2017.
- Caneiro JP. Braz J Phys Ther 2021.
- Caneiro JP. Phys Ther 2022.
- Launer J. Narrative based practice in health and social care: conversations inviting change. 2018. Routledge, London.
- Hutting N. J Orthop Sports Phys Ther 2019.
- Hutting N. Musculoskelet Sci Pract 2022.