Manuela Deodato (Department of Medical, Surgical and Health Sciences, University of Trieste, Trieste, Italy )
Migraine represents a common neurologic condition that leads to adverse effects on physical/cognitive functioning and to a considerable socioeconomic burden among many countries1. On the one side, part of this burden is due to multiple comorbidities that increased the headache-related disability2. On the other side, part of this burden is due to its complex physiopathology that is still an object of studies for a better understanding of underlying mechanisms and for a better choice of its treatments3. Neurophysiology studies have established that migraine is “a brain state of altered excitability” in a “migraine brain” genetically predisposed3,4. In fact, migraine people present a general increase response to sensory stimuli due to two opposing processes: lack of habituation and sensitization4. The aim of this PhD project was to investigate the effects of two emerging pharmacological and non-pharmacological treatments with respect to habituation and sensitization outcomes.
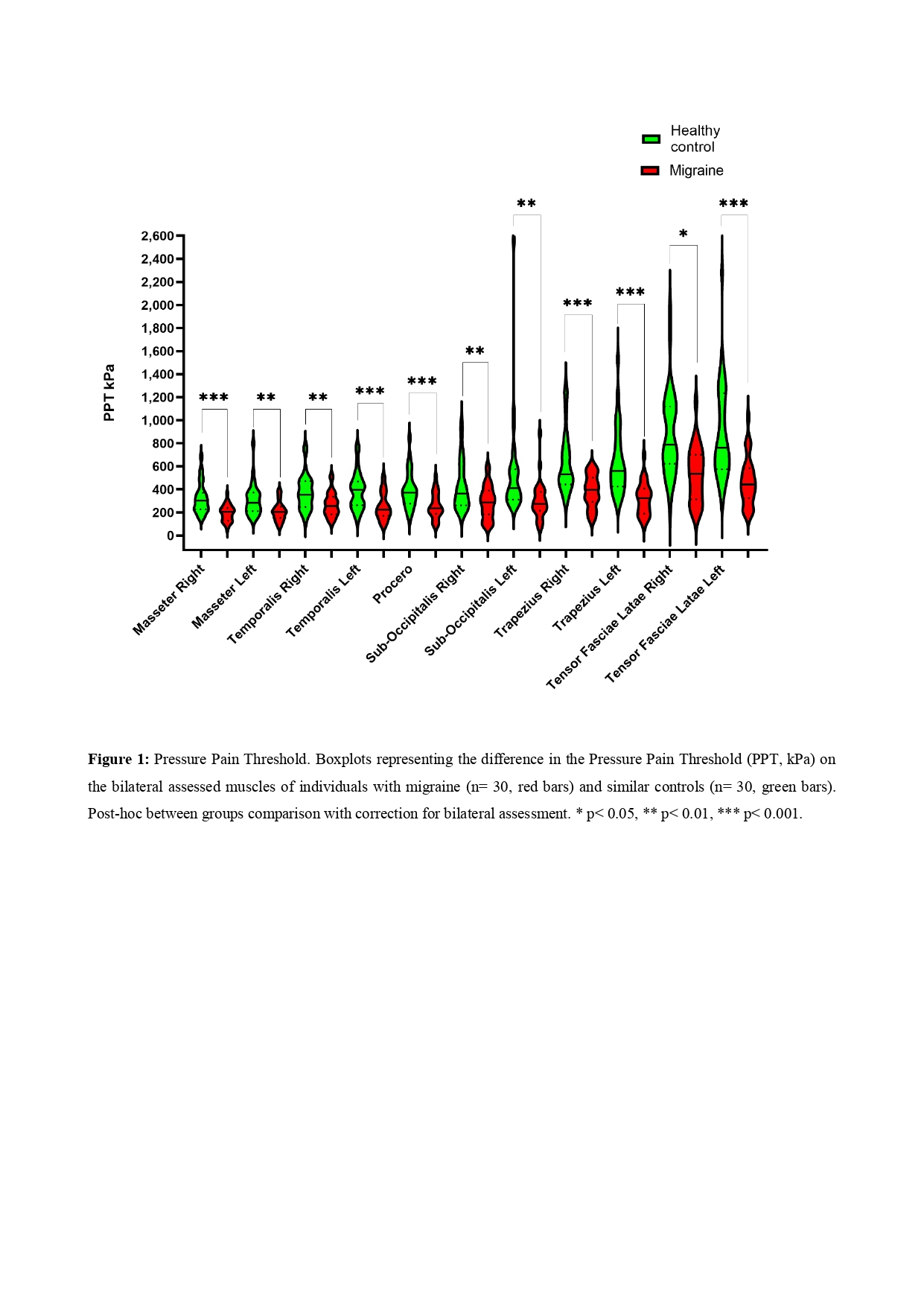
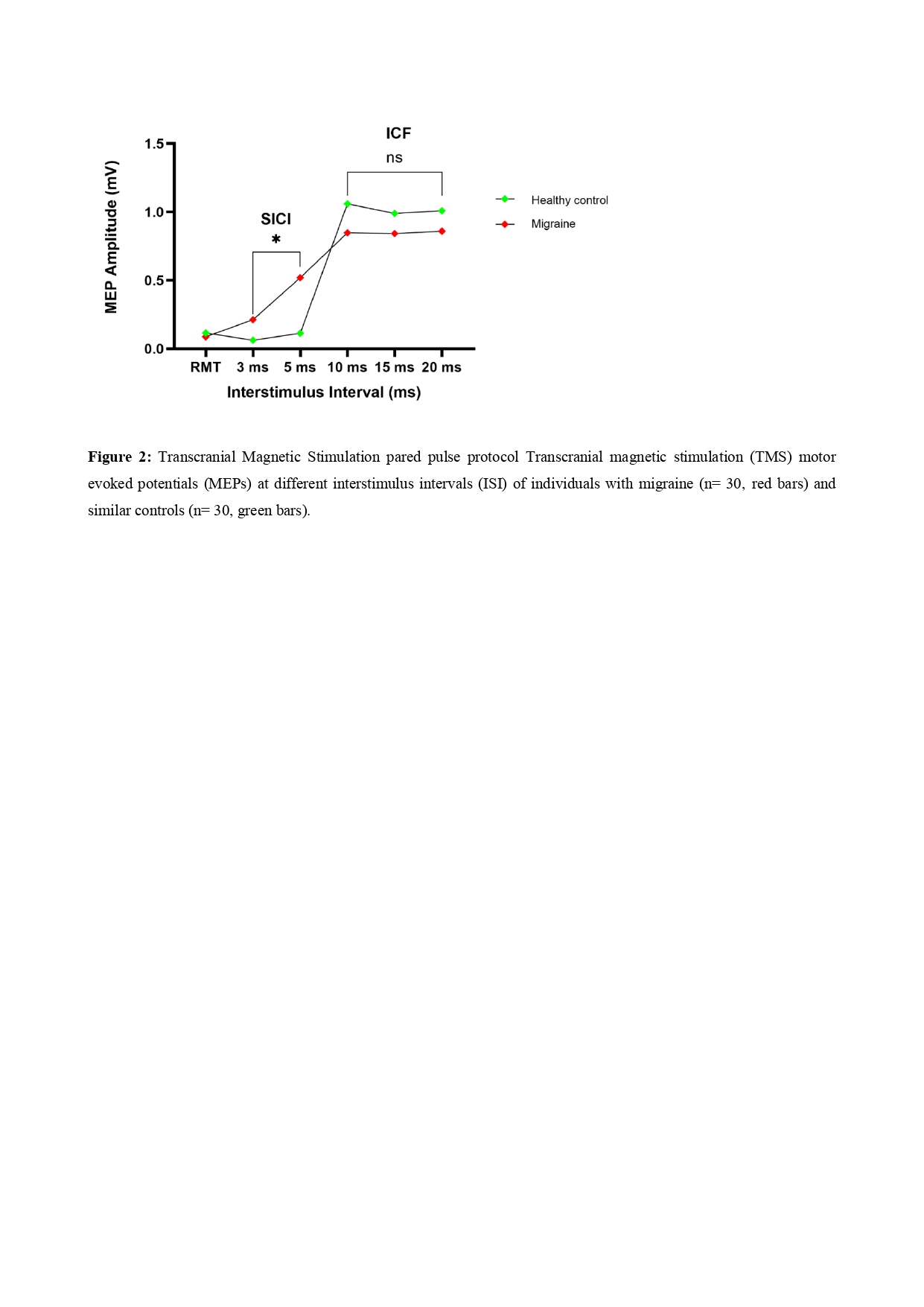
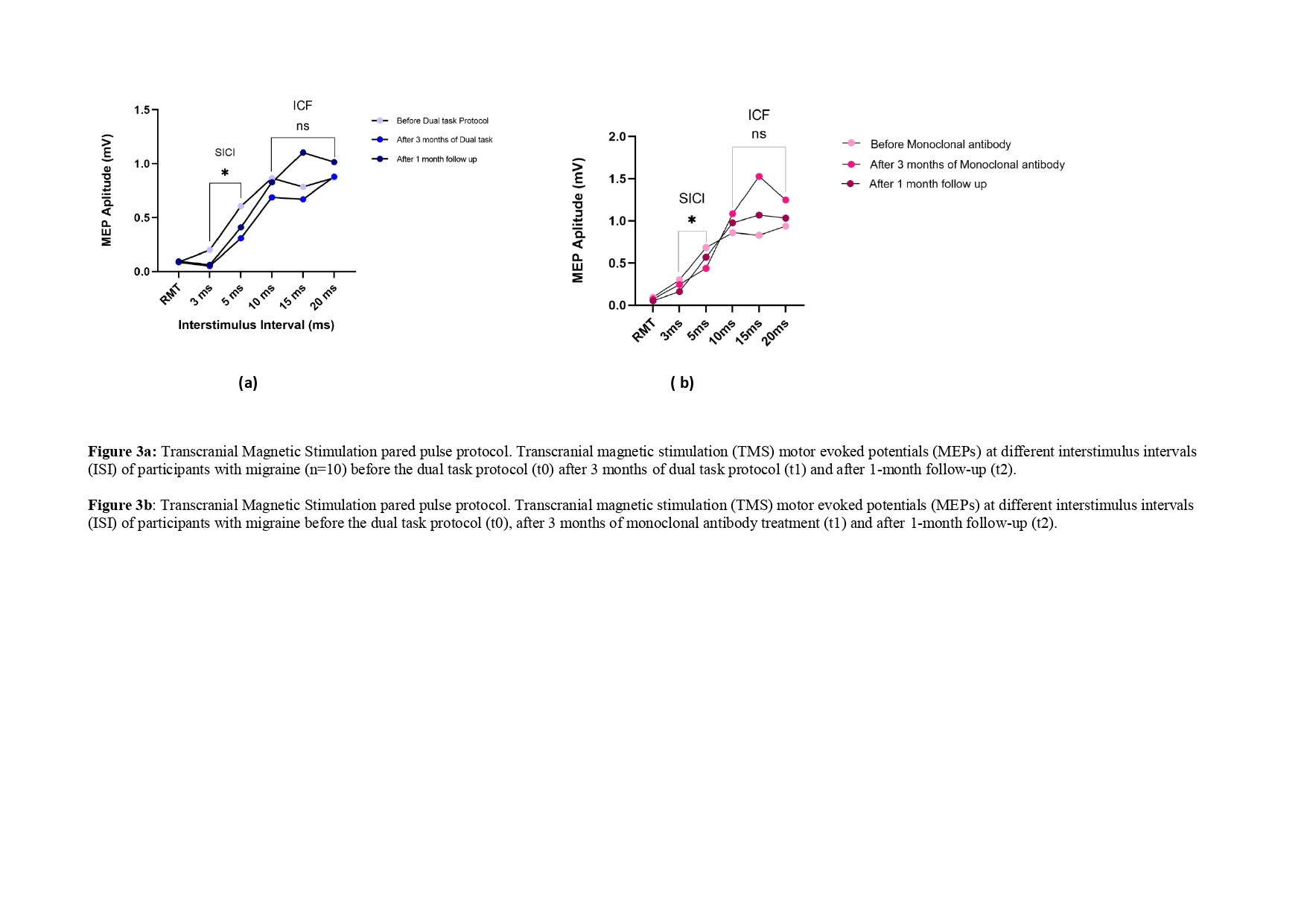
Three studies were conducted. In each study, the same neurophysiologic and clinical habituation and sensitization outcomes were used: Algometer assessment, Transcranial Magnetic stimulation, Neuropsychological tests on executive functions, the Migraine Disability Assessment Scale and headache diary.
1) Study 1, a cross sectional study, compared habituation and sensitization outcomes in 30 migraine people with respect to 30 healthy controls.
2) Study 2, a randomized control trial, compared the dual task protocol in migraine people with active exercise only and with cognitive training only, concerning habituation and sensitization outcomes (3 months of each treatments plus 1-month follow-up).
3) Study 3, an observational study, compared the two emerging pharmacological and non-pharmacological treatments, respectively, monoclonal antibody and dual task protocol, on habituation and sensitization outcomes (3 months of each treatments plus 1-month follow-up).
Study 1 reported that people with migraine were characterized by a statistically significant alteration of all habituation/sensitization neurophysiological and clinical outcomes with respect to healthy controls. Study 2 suggested that active exercise was useful in sensitization outcomes, while cognitive training in habituation outcomes. As a consequence, the Dual task protocol resulted more useful than two monotherapies, active exercise and cognitive training alone, through a more evident effects on habituation and sensitization outcomes. Finally, Study 3 shows similar general peripheral and central effects of both dual task protocol and monoclonal antibody treatments in patients with migraine. However, monoclonal antibody therapy seems to be more useful for some sensitization outcomes (reduction of drug intake, migraine frequency and migraine responders rates) while dual task protocol seems to be more useful for habituation outcomes (improvement in intracortical inhibition).
Taken together, the findings from these three studies suggest the coexistence of both central and peripheral adaptive neurophysiological mechanisms in people with migraine that can be objectively measured with validated techniques5. Such techniques can also be useful to evaluate the efficacy of different therapies: our preliminary results suggest that non-pharmacological interventions, such as physiotherapy, can significantly improve habituation and sensitization outcomes in this patients’ population. Particularly, a dual task protocol, active exercise with concomitant cognitive training, may up-regulate the cortical connectivity related to cognitive task due to an activity-dependent learning that increase the synaptic strength and promote the associative learning and neuroplasticity6. Future studies could include the effect of the combination of both monoclonal antibody and dual task protocols on habituation and sensitization outcomes.