Riabilitazione precoce con realtà aumentata e gamification dopo intervento chirurgico in pazienti con frattura di arto inferiore
Early rehabilitation program with augmented reality and gamification after surgery in patients with lower limb fractures
Introduction
The rehabilitative pathway following surgery for lower limb fracture can be lengthy, significantly impacting both quality of life and work [ 1 ]. Weight-bearing guidelines are dependent on the operating surgeon, and typically, physiotherapy and functional retraining begin after a period of immobilization and weight-bearing restriction.
After this period, patients often tend to underutilize the affected limb in functional tasks due to movement-related fear [ 2 ] or excessive control over the injured limb.
Incorporating immersive and gamified exercise through augmented reality allows patients to shift the load correctly between both lower limbs. The challenging context serves as a catalyst in increasing patient’s motivation to achieve their goals [ 3 ]. Furthermore, rehabilitation exergames contribute to increase patient engagement, thereby reducing the repetitiveness of the exercises.
Methods
Nineteen patients, ranging in age from 18 to 65 years, without severe comorbidities, and who were permitted early weight-bearing after surgery, were enrolled in the study.
Eleven patients (control group) followed the standard rehabilitation protocol provided by the regional healthcare system, which included traditional physiotherapy. Conversely, eight patients (study group) participated in an early rehabilitation program (started on average 5 days post-surgery) that incorporated physiotherapy with exercises using the D-Wall Tecnobody® system. The exergames involved controlled weight transfers through pelvic movement, as well as the simulation of more complex gestures with the upper limbs, requiring proper control of the base of support.
At 6 weeks and 3 months post-surgery, functional clinical questionnaires were administered. Simultaneously, the return to autonomy, work, and sports activities were investigated.
Results
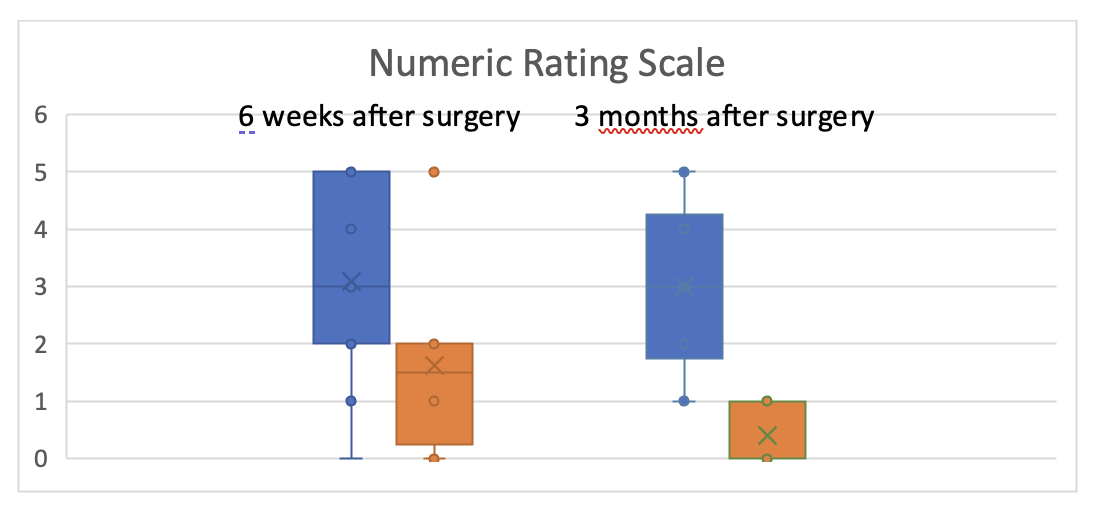
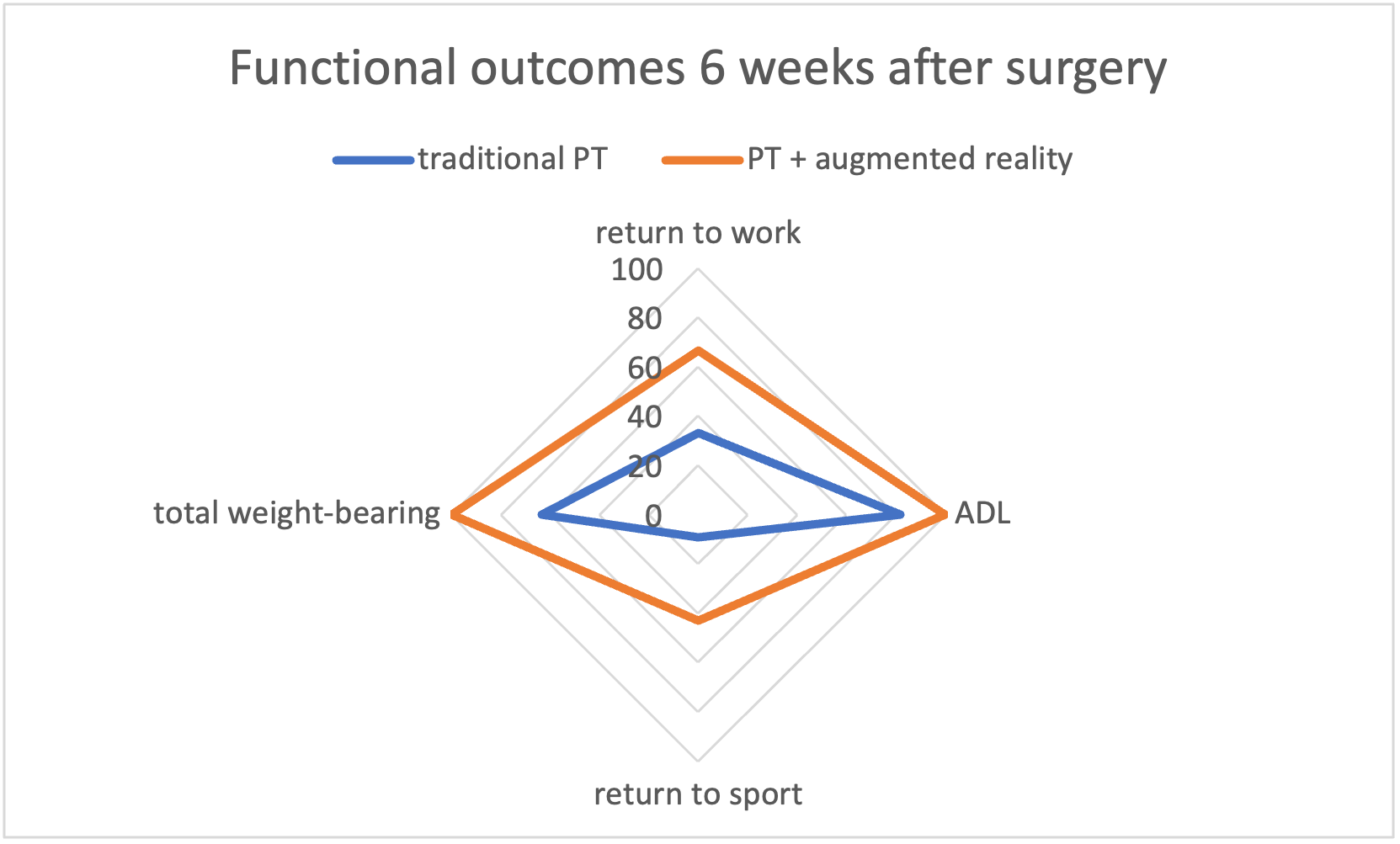
At 6 weeks, the study group achieved complete (100%) return to full weight-bearing and autonomy, while 63% of patients in control group achieved full weight-bearing and 81% autonomy. In the study group, 66% had returned to work and 42% to sports activities, compared to 33% returning to work and 9% returning to sports in the control group. The groups showed statistical differences in NRS (p-value 0,046) and WOMAC (p-value 0,0013) questionnaires, with better scores in the study group. At 3 months, the difference between groups persisted in NRS score (p-value 0,0025), while the results of other questionnaires aligned, indicating functional recovery in both groups. No complications occurred.
Overall, patients undergoing early physiotherapy intervention had an average of 11.42 physiotherapy treatments, while patients in the control group required the prescription of multiple physiotherapy session to achieve complete recovery, with an average of 28.18 (p-value 0,0012).
Discussion and Conclusion
The availability of current rehabilitation technologies, such as gamified exercises in augmented reality, offers the opportunity to transform traditional physiotherapy into a dynamic process. This allows patients to gain immediate awareness of the load-bearing possibilities on the operated limb within more complex movements, without developing protective mechanisms or avoiding the use of the fractured limb. This has the potential to decrease the inactivity period, the number of prescribed physiotherapy sessions, and the economic impact for patients receiving early weight-bearing recommendations after surgery.
REFERENCES
[ 1 ] Black JDJ et al., Early weight-bearing in operatively fixed ankle fractures: A systematic review, The Foot, 2013;23(2):78–85
[ 2 ] Steven JL et al., Pain-related fear, catastrophizing and pain in the recovery from a fracture, Scandinavian Journal of Pain, 2010 ;1(1):38–42
[ 3 ] S. Sandrone et al., Gamification and game-based education in neurology and neuroscience: application, challenges and opportunities, Brain Disorders, Vol. 1, 2021, 100008, ISSN 2666-4593